Table Of Contents
Category
Artificial Intelligence (AI)
Machine Learning (ML)
Natural Language Processing (NLP)
Cloud Computing
Blockchain
Blockchain-as-a-Service (BaaS)
1. Introduction to Rare Disease Diagnostics
Rare diseases, often defined as conditions affecting fewer than 200,000 individuals in the United States, pose significant challenges in diagnosis and treatment. With over 7,000 known rare diseases, many remain undiagnosed or misdiagnosed due to their complexity and the limited knowledge surrounding them.
- Prevalence and Impact: Approximately 1 in 10 Americans is affected by a rare disease at some point in their lives. Many rare diseases are genetic, chronic, and life-threatening, leading to a substantial burden on patients and healthcare systems.
- Challenges in Diagnosis:
- Limited Awareness: Healthcare professionals may lack familiarity with specific rare diseases, leading to delays in diagnosis.
- Diverse Symptoms: Symptoms can vary widely, often overlapping with more common conditions, complicating the diagnostic process.
- Access to Expertise: Specialists in rare diseases are often scarce, making it difficult for patients to receive timely and accurate diagnoses.
- Importance of Early Diagnosis: Early and accurate diagnosis can significantly improve patient outcomes by allowing for timely interventions, which can enhance quality of life and reduce healthcare costs.
- Role of Technology: Advances in technology, particularly artificial intelligence (AI), are transforming the landscape of rare disease diagnostics. AI can analyze vast amounts of data, identify patterns, and assist healthcare professionals in making informed decisions. At Rapid Innovation, we leverage AI to develop tailored solutions that enhance diagnostic processes, ultimately leading to improved patient outcomes and greater return on investment for healthcare providers. Learn more about how AI agents can support diagnostics in our AI agents for diagnostic support.
In summary, the landscape of rare disease diagnostics is fraught with challenges, but the integration of AI technology holds promise for improving diagnostic accuracy and patient care. Rapid Innovation is committed to helping clients navigate these complexities, ensuring they achieve their business goals efficiently and effectively.
1.1. The Challenge of Rare Disease Identification
Identifying rare diseases presents a significant challenge for healthcare professionals and researchers. Rare diseases, defined as conditions affecting fewer than 200,000 individuals in the United States, often go undiagnosed or misdiagnosed due to their low prevalence and the complexity of symptoms.
- Limited Awareness: Many healthcare providers may not be familiar with rare diseases, leading to delayed or incorrect diagnoses.
- Symptom Overlap: Rare diseases often share symptoms with more common conditions, complicating the diagnostic process.
- Genetic Complexity: Many rare diseases are genetic, involving mutations that can vary widely even among patients with the same condition.
- Data Scarcity: There is often a lack of comprehensive data on rare diseases, making it difficult to establish clear diagnostic criteria.
- Patient Advocacy: Patients and families may struggle to find support and information, leading to feelings of isolation and frustration.
The challenge of rare disease identification is compounded by the need for specialized knowledge and resources, which are often limited in standard healthcare settings.
1.2. Current Diagnostic Landscape and Limitations

The current diagnostic landscape for rare diseases is characterized by a combination of traditional methods and emerging technologies, but it still faces significant limitations.
- Diagnostic Tests: Many rare diseases require specific genetic tests or biomarkers for accurate diagnosis, which may not be readily available.
- Time-Consuming Processes: Diagnosing a rare disease can take years, as patients often undergo multiple tests and consultations before receiving a definitive diagnosis.
- High Costs: Genetic testing and specialized consultations can be expensive, creating barriers for many patients.
- Limited Access: Not all healthcare facilities have access to the latest diagnostic technologies, leading to disparities in care.
- Fragmented Data: Patient data is often siloed, making it difficult to share information across healthcare systems and hindering research efforts.
These limitations highlight the need for more efficient and accessible diagnostic solutions in the realm of rare diseases.
1.3. The Promise of AI in Rare Disease Detection
Artificial Intelligence (AI) holds great promise for improving the detection and diagnosis of rare diseases. By leveraging advanced algorithms and machine learning, AI can enhance the diagnostic process in several ways.
- Data Analysis: AI can analyze vast amounts of patient data, identifying patterns and correlations that may not be apparent to human clinicians. Rapid Innovation specializes in developing AI-driven solutions that empower healthcare providers to make informed decisions based on comprehensive data insights.
- Speed and Efficiency: AI algorithms can process information quickly, potentially reducing the time it takes to reach a diagnosis. Our solutions are designed to streamline workflows, enabling healthcare professionals to focus on patient care rather than administrative tasks.
- Predictive Analytics: Machine learning models can predict the likelihood of a rare disease based on patient symptoms and genetic information, guiding clinicians toward the most relevant tests. Rapid Innovation's predictive analytics tools help healthcare providers prioritize testing and treatment options, ultimately improving patient outcomes.
- Enhanced Imaging: AI can improve the interpretation of medical imaging, helping to identify subtle signs of rare diseases that may be missed by the human eye. Our advanced imaging solutions assist radiologists in making more accurate diagnoses, reducing the risk of oversight.
- Collaboration and Sharing: AI can facilitate data sharing among researchers and healthcare providers, fostering collaboration and accelerating the discovery of new diagnostic criteria. Rapid Innovation's platforms promote seamless communication and data exchange, enhancing research efforts in the rare disease space.
The integration of AI into the diagnostic landscape for rare diseases has the potential to transform patient care, making it more accurate, timely, and accessible. By partnering with Rapid Innovation, healthcare organizations can leverage cutting-edge AI technologies to achieve greater ROI and improve the overall quality of care for patients with rare diseases.
1.4. Ethical and Regulatory Considerations
Ethical and regulatory considerations are paramount in the development and deployment of technologies in healthcare, particularly in areas like artificial intelligence (AI) and machine learning (ML). These considerations ensure that innovations are not only effective but also safe, equitable, and respectful of patient rights.
- Patient Privacy: Protecting patient data is crucial. Regulations like HIPAA in the U.S. mandate strict guidelines on how personal health information is handled. Ensuring data anonymization and secure storage is essential to maintain trust, which is a core value at Rapid Innovation. The use of artificial intelligence in healthcare must prioritize patient privacy to comply with these regulations.
- Informed Consent: Patients should be fully informed about how their data will be used, especially in AI training. Clear communication about the implications of data sharing is necessary to uphold ethical standards, and Rapid Innovation emphasizes this in its consulting practices. This is particularly important in the context of artificial intelligence in healthcare, where data is often utilized for training AI medical diagnosis systems.
- Bias and Fairness: AI systems can inadvertently perpetuate biases present in training data. It is vital to ensure that algorithms are trained on diverse datasets to avoid discrimination against certain groups. Regular audits and updates can help mitigate these risks, a service Rapid Innovation provides to its clients to enhance their AI solutions. This is especially relevant in the field of artificial intelligence in medical diagnosis, where biased data can lead to unequal treatment outcomes.
- Accountability: Establishing clear lines of accountability is essential when AI systems make diagnostic or treatment recommendations. Determining who is responsible for errors—whether it be the developers, healthcare providers, or institutions—can be complex but is necessary for ethical practice. Rapid Innovation assists organizations in defining these accountability frameworks, particularly in the context of artificial intelligence in healthcare.
- Regulatory Compliance: Adhering to regulations set by bodies like the FDA or EMA is critical. These organizations provide guidelines for the approval and monitoring of AI technologies in healthcare, ensuring they meet safety and efficacy standards. Rapid Innovation helps clients navigate these regulatory landscapes effectively, particularly in the rapidly evolving field of artificial intelligence in healthcare management.
- Transparency: AI systems should be transparent in their decision-making processes. This includes providing explanations for how diagnoses or treatment recommendations are made, which can help healthcare providers and patients understand and trust the technology. Rapid Innovation advocates for transparency in all AI implementations, especially in the context of artificial intelligence in healthcare articles and research.
- Continuous Monitoring: Post-deployment monitoring of AI systems is essential to ensure they perform as intended and do not cause harm. This includes tracking outcomes and making necessary adjustments based on real-world data. Rapid Innovation offers ongoing support to ensure that AI systems remain compliant and effective, particularly in the context of AI patient monitoring and artificial intelligence use in healthcare. For more information on how we can assist you, learn more about AI and ML uses and future insights.
2. Foundational Technologies
Foundational technologies are the building blocks that enable advancements in various fields, including healthcare. In the context of medical diagnostics, several key technologies play a crucial role in enhancing the accuracy and efficiency of diagnoses.
- Artificial Intelligence (AI): AI encompasses a range of technologies that simulate human intelligence. In medical diagnostics, AI can analyze vast amounts of data quickly, identifying patterns that may not be visible to human practitioners. This includes applications such as artificial intelligence in healthcare and AI medical diagnosis.
- Machine Learning (ML): A subset of AI, ML involves algorithms that learn from data. In healthcare, ML models can improve over time, becoming more accurate as they are exposed to more patient data. This is particularly relevant in the context of artificial intelligence in healthcare companies that utilize machine learning for improved patient outcomes.
- Natural Language Processing (NLP): NLP allows computers to understand and interpret human language. In medical diagnostics, NLP can be used to analyze clinical notes, research papers, and patient records, extracting valuable insights for better decision-making. This technology is increasingly being integrated into artificial intelligence in healthcare applications.
- Big Data Analytics: The ability to process and analyze large datasets is crucial in healthcare. Big data analytics can identify trends, predict outcomes, and support personalized medicine by analyzing patient histories and treatment responses. This is particularly relevant for artificial intelligence in healthcare market trends.
- Cloud Computing: Cloud technology enables the storage and processing of large volumes of data remotely. This facilitates collaboration among healthcare providers and researchers, allowing for real-time data sharing and analysis, which is essential for the implementation of AI in healthcare examples.
- Internet of Medical Things (IoMT): IoMT refers to connected devices that collect and transmit health data. These devices can provide continuous monitoring of patients, leading to timely interventions and improved outcomes, aligning with the goals of AI patient monitoring.
- Blockchain Technology: Blockchain can enhance data security and integrity in healthcare. By providing a decentralized and tamper-proof ledger, it ensures that patient records are secure and accessible only to authorized individuals, which is crucial for maintaining trust in artificial intelligence in healthcare.
2.1. Machine Learning Architectures for Medical Diagnostics
Machine learning architectures are essential for developing effective diagnostic tools in healthcare. These architectures determine how data is processed and analyzed, impacting the accuracy and reliability of diagnostic outcomes.
- Supervised Learning: This architecture involves training models on labeled datasets, where the input data is paired with the correct output. In medical diagnostics, supervised learning can be used to classify diseases based on patient symptoms and test results, a common application in artificial intelligence in medical diagnosis.
- Unsupervised Learning: Unlike supervised learning, unsupervised learning deals with unlabeled data. It can identify hidden patterns or groupings in data, which can be useful for discovering new disease subtypes or patient clusters, relevant in the context of artificial intelligence in healthcare.
- Deep Learning: A subset of ML, deep learning uses neural networks with multiple layers to analyze complex data. In medical imaging, deep learning algorithms can detect anomalies in X-rays, MRIs, and CT scans with high accuracy, showcasing the potential of artificial intelligence in healthcare.
- Reinforcement Learning: This architecture involves training models through trial and error, receiving feedback based on their actions. In diagnostics, reinforcement learning can optimize treatment plans by learning from patient responses over time, a promising area for AI in healthcare.
- Ensemble Learning: This approach combines multiple models to improve predictive performance. By aggregating the strengths of different algorithms, ensemble learning can enhance diagnostic accuracy and reduce the likelihood of errors, which is critical for artificial intelligence in medical diagnosis.
- Transfer Learning: Transfer learning allows models trained on one task to be adapted for another. In medical diagnostics, this can be particularly useful when there is limited data available for a specific condition, leveraging knowledge from related areas, a technique often used in artificial intelligence in healthcare.
- Generative Adversarial Networks (GANs): GANs consist of two neural networks that compete against each other to generate new data. In healthcare, GANs can be used to create synthetic medical images for training purposes, helping to augment datasets and improve model performance, which is a significant advancement in artificial intelligence in healthcare.
By leveraging these machine learning architectures, healthcare providers can enhance diagnostic accuracy, leading to better patient outcomes and more efficient healthcare delivery. Rapid Innovation is committed to helping clients implement these technologies effectively, ensuring they achieve greater ROI and improved patient care through the use of artificial intelligence in healthcare.
2.2. Natural Language Processing in Clinical Documentation

Natural Language Processing (NLP) is revolutionizing clinical documentation by enabling healthcare professionals to efficiently manage and analyze vast amounts of unstructured data. This technology allows for the extraction of meaningful information from clinical notes, patient records, and other textual data sources, including medical natural language processing and healthcare natural language processing.
- Enhances data entry: NLP tools can automate the transcription of spoken words into written text, significantly reducing the time healthcare providers spend on documentation. This efficiency translates into more time for patient care, ultimately improving service delivery. Applications of NLP in healthcare are becoming increasingly prevalent.
- Improves accuracy: By utilizing algorithms that understand medical terminology, NLP minimizes errors in clinical documentation, ensuring that patient records are precise and reliable. This accuracy is crucial for maintaining high standards of patient safety and care, particularly in medical NLP.
- Facilitates information retrieval: NLP enables quick access to relevant patient information, allowing healthcare providers to make informed decisions based on comprehensive data analysis. This capability enhances the overall quality of care and supports better patient outcomes, as seen in various NLP use cases in healthcare.
- Supports clinical decision-making: By analyzing patient notes and histories, NLP can identify patterns and suggest potential diagnoses or treatment options. This analytical support empowers healthcare professionals to make timely and informed decisions, showcasing the importance of NLP applications in healthcare.
- Streamlines coding and billing: NLP can assist in the coding process by automatically identifying relevant codes from clinical documentation, improving billing accuracy and efficiency. This not only enhances revenue cycle management but also reduces administrative burdens, making NLP solutions for healthcare essential.
The integration of NLP in clinical documentation not only enhances the quality of patient care but also optimizes administrative processes within healthcare organizations, leading to greater operational efficiency and improved return on investment (ROI). The rise of healthcare NLP tools and companies is indicative of this trend.
2.3. Computer Vision for Medical Imaging Analysis
Computer Vision (CV) is a branch of artificial intelligence that enables machines to interpret and understand visual information from the world. In the medical field, CV is increasingly being used for medical imaging analysis, providing significant advancements in diagnostics and treatment planning.
- Automated image analysis: CV algorithms can analyze medical images such as X-rays, MRIs, and CT scans, identifying abnormalities with high accuracy and speed. This automation reduces the workload on radiologists and accelerates the diagnostic process.
- Early detection of diseases: By recognizing patterns in imaging data, CV can assist in the early detection of conditions like cancer, leading to timely interventions and improved patient outcomes. Early detection is critical for effective treatment and can significantly enhance survival rates.
- Enhanced diagnostic support: CV tools can provide radiologists with second opinions, reducing the likelihood of missed diagnoses and improving overall diagnostic accuracy. This collaborative approach fosters a more reliable diagnostic environment.
- Workflow efficiency: Automating image analysis allows healthcare professionals to focus on patient care rather than manual image interpretation, streamlining workflows in radiology departments. This efficiency can lead to cost savings and improved patient throughput.
- Integration with electronic health records: CV can be integrated with EHR systems, allowing for seamless access to imaging data alongside patient histories, enhancing clinical decision-making. This integration supports a more holistic view of patient health.
The application of computer vision in medical imaging is transforming the landscape of diagnostics, making it faster and more reliable, ultimately contributing to enhanced patient care and operational efficiency.
2.4. Multi-modal Data Integration Frameworks
Multi-modal data integration frameworks are essential in healthcare as they enable the combination of diverse data types from various sources, including structured data (like lab results) and unstructured data (like clinical notes). This integration is crucial for comprehensive patient care and advanced analytics.
- Holistic patient view: By integrating data from multiple modalities, healthcare providers can gain a complete understanding of a patient's health status, leading to more personalized treatment plans. This comprehensive view is vital for tailoring interventions to individual patient needs.
- Improved predictive analytics: Multi-modal frameworks allow for the analysis of complex datasets, enhancing the ability to predict patient outcomes and identify at-risk populations. This predictive capability supports proactive healthcare management.
- Enhanced research capabilities: Researchers can leverage integrated data to uncover insights that may not be apparent when analyzing single data types, driving innovation in medical research. This innovation can lead to breakthroughs in treatment and care methodologies.
- Streamlined data management: These frameworks facilitate the organization and retrieval of data from various sources, improving efficiency in healthcare operations. Efficient data management is essential for maintaining high-quality patient care.
- Support for machine learning applications: Multi-modal data integration is critical for training machine learning models, as it provides the diverse datasets needed for accurate predictions and analyses. This capability enhances the potential for AI-driven solutions in healthcare.
The development of multi-modal data integration frameworks is pivotal in advancing healthcare analytics, ultimately leading to improved patient care and operational efficiency. Rapid Innovation is committed to helping healthcare organizations implement these advanced technologies, ensuring they achieve their business goals effectively and efficiently.
2.5. Knowledge Representation for Medical Ontologies
Knowledge representation in medical ontologies is crucial for organizing and sharing medical knowledge effectively. It involves the use of structured frameworks that allow for the representation of complex medical concepts and their relationships. Medical ontologies, including healthcare ontologies, provide a common vocabulary for healthcare professionals, enabling better communication and understanding. They facilitate the integration of diverse data sources, improving interoperability among different healthcare systems. Ontologies can represent various medical concepts, including diseases, symptoms, treatments, and patient demographics. By using formal languages like OWL (Web Ontology Language) and RDF (Resource Description Framework), medical ontologies can be machine-readable, allowing for automated reasoning and knowledge discovery. Examples of widely used medical ontologies include SNOMED CT, LOINC, and the Gene Ontology, which help standardize terminology across different healthcare settings. The development of these ontologies often involves collaboration among clinicians, researchers, and informaticians to ensure they accurately reflect current medical knowledge and practices.
At Rapid Innovation, we leverage our expertise in AI to assist healthcare organizations in developing and implementing robust medical ontologies. By creating tailored ontologies, we help clients enhance their data interoperability and improve clinical decision-making processes, ultimately leading to greater ROI through more efficient patient care. Our MLOps consulting services can further support these initiatives by ensuring that the underlying machine learning models are effectively integrated and managed.
3. Data Requirements and Management
Effective data management is essential in healthcare to ensure that clinical data is accurate, accessible, and secure. This involves understanding the data requirements for various healthcare applications and implementing strategies for data management. Data quality is paramount; it must be accurate, complete, and timely to support clinical decision-making. Data governance frameworks should be established to ensure compliance with regulations such as HIPAA and GDPR. Data storage solutions must be scalable to accommodate the growing volume of healthcare data generated daily. Data management practices should include regular audits and validation processes to maintain data integrity.
3.1. Clinical Data Sources and Integration
Clinical data sources are diverse and include electronic health records (EHRs), laboratory information systems, imaging systems, and patient-generated data. Integrating these sources is vital for comprehensive patient care and research. EHRs are a primary source of clinical data, containing patient demographics, medical history, medications, and treatment plans. Laboratory information systems provide critical data on test results, which are essential for diagnosis and treatment. Imaging systems contribute valuable visual data, such as X-rays and MRIs, which can be integrated with other clinical information for a holistic view of patient health. Patient-generated data, including wearable device data and patient-reported outcomes, can enhance clinical insights and support personalized medicine. Integration challenges include data standardization, ensuring interoperability among different systems, and addressing privacy concerns. Utilizing health information exchanges (HIEs) can facilitate the sharing of clinical data across different healthcare organizations, improving care coordination and outcomes. Advanced technologies like APIs (Application Programming Interfaces) and FHIR (Fast Healthcare Interoperability Resources) are increasingly used to streamline data integration processes.
At Rapid Innovation, we specialize in developing comprehensive data management strategies that address these integration challenges. Our AI-driven solutions enable seamless data integration across various clinical sources, ensuring that healthcare organizations can deliver high-quality care while maximizing their operational efficiency and ROI.
By focusing on these aspects of knowledge representation and data management, healthcare organizations can enhance their ability to deliver high-quality care and leverage data for improved patient outcomes.
3.1.1. Electronic Health Records (EHR)

Electronic Health Records (EHR) are digital versions of patients' paper charts. They are real-time, patient-centered records that make information available instantly and securely to authorized users. EHRs, including medical electronic record systems and electronic healthcare record systems, are designed to streamline the clinician's workflow and improve the quality of care.
- Comprehensive patient information: EHRs contain a wide range of data, including medical history, medications, allergies, lab test results, and treatment plans. This comprehensive data repository allows healthcare providers to make informed decisions quickly, ultimately enhancing patient outcomes.
- Enhanced coordination of care: EHRs facilitate better communication among healthcare providers, ensuring that all members of a patient's care team have access to the same information. This interconnectedness is crucial for delivering coordinated care, which can lead to improved patient satisfaction and reduced costs.
- Improved patient safety: EHRs can reduce errors related to handwriting or transcription, and they often include clinical decision support tools that alert providers to potential issues, such as drug interactions. By leveraging AI algorithms, Rapid Innovation can enhance these decision support systems, further minimizing risks and improving patient safety.
- Increased efficiency: EHRs can automate administrative tasks, such as scheduling and billing, allowing healthcare providers to focus more on patient care. Rapid Innovation can implement AI-driven automation solutions that optimize these processes, leading to significant time and cost savings.
- Regulatory compliance: EHRs help healthcare organizations comply with regulations, such as the Health Insurance Portability and Accountability Act (HIPAA), by ensuring that patient information is stored securely. Our expertise in AI can further enhance data security measures, ensuring compliance while protecting sensitive information.
3.1.2. Laboratory Test Results
Laboratory test results are critical components of patient care, providing essential information for diagnosis, treatment, and monitoring of health conditions. The integration of lab results into EHR systems, including electronic medical record systems and medical EMR systems, has transformed how healthcare providers access and utilize this information.
- Timely access to results: EHRs allow healthcare providers to receive lab results in real-time, enabling quicker decision-making and treatment adjustments. Rapid Innovation can develop predictive analytics tools that help providers anticipate patient needs based on lab results.
- Improved accuracy: Electronic transmission of lab results reduces the risk of errors associated with manual entry or miscommunication. Our AI solutions can further enhance the accuracy of data interpretation, ensuring that healthcare providers have the most reliable information at their fingertips.
- Comprehensive data analysis: EHRs can aggregate lab results over time, allowing providers to track changes in a patient's health status and make informed decisions based on trends. Rapid Innovation can implement advanced data analytics to uncover insights that drive better clinical outcomes.
- Enhanced patient engagement: Patients can access their lab results through patient portals, promoting transparency and encouraging them to take an active role in their healthcare. Our AI-driven engagement tools can personalize communication, fostering a stronger patient-provider relationship.
- Streamlined workflows: EHRs can automate the ordering of lab tests and the retrieval of results, reducing administrative burdens on healthcare staff. Rapid Innovation can optimize these workflows with AI, ensuring that healthcare teams operate at peak efficiency.
3.1.3. Medical Imaging
Medical imaging encompasses various techniques used to visualize the interior of the body for clinical analysis and medical intervention. The integration of medical imaging into EHR systems has significantly improved the efficiency and effectiveness of patient care.
- Diverse imaging modalities: Medical imaging includes X-rays, MRIs, CT scans, and ultrasounds, each providing unique insights into a patient's health. Rapid Innovation can develop AI algorithms that enhance image analysis, leading to more accurate diagnoses.
- Centralized access: EHRs allow healthcare providers to access medical imaging results alongside other patient information, facilitating a more comprehensive understanding of a patient's condition. Our solutions can ensure seamless integration of imaging data into EHRs, enhancing the clinician's workflow.
- Enhanced diagnostic accuracy: The ability to view imaging results in conjunction with lab results and clinical notes helps providers make more accurate diagnoses. Rapid Innovation's AI tools can assist in identifying patterns in imaging data, further improving diagnostic precision.
- Improved collaboration: EHRs enable radiologists and other specialists to share imaging results and collaborate on patient care more effectively. Our collaborative platforms can enhance communication among care teams, ensuring that all stakeholders are aligned in their approach to patient care.
- Reduced duplication of tests: By having access to a patient's imaging history, providers can avoid unnecessary repeat tests, saving time and resources. Rapid Innovation can implement AI-driven solutions that flag redundant tests, optimizing resource utilization.
In conclusion, the integration of Electronic Health Records, including medical practice EHR and electronic medical records, laboratory test results, and medical imaging into healthcare systems has revolutionized patient care. These technologies enhance communication, improve accuracy, and streamline workflows, ultimately leading to better health outcomes. Rapid Innovation is committed to leveraging AI to further enhance these systems, helping healthcare organizations achieve greater ROI and improved patient care.
3.1.4. Genetic and Genomic Data
Genetic and genomic data play a crucial role in understanding the biological basis of diseases, particularly in the fields of personalized medicine and genomics. This data encompasses a wide range of information, including:
- DNA sequences: The complete sequence of nucleotides in an organism's genome, which can reveal mutations associated with diseases.
- Gene expression profiles: Information on how genes are expressed in different tissues or conditions, helping to identify which genes are active in specific diseases.
- Genetic variants: Variations in DNA sequences, such as single nucleotide polymorphisms (SNPs), that can influence an individual's susceptibility to diseases.
The integration of genetic and genomic data with other types of data, such as clinical and environmental data, enhances the understanding of complex diseases. This multi-omics approach allows researchers to identify biomarkers for early diagnosis and treatment strategies tailored to individual patients.
However, the analysis of genetic and genomic data presents challenges, including:
- Data complexity: The sheer volume and complexity of genomic data require advanced computational tools and bioinformatics expertise, areas where Rapid Innovation excels. Our AI-driven solutions can streamline data processing, enabling clients to derive actionable insights more efficiently. This includes services like raw dna data analysis and whole exome testing.
- Ethical considerations: Issues related to privacy, consent, and the potential for genetic discrimination must be addressed when handling genetic data. Rapid Innovation provides consulting services to help clients navigate these ethical landscapes, ensuring compliance and fostering trust.
3.2. Data Quality and Preprocessing Techniques
Data quality is paramount in any research, especially in fields like healthcare and genomics where decisions can have significant implications. Ensuring high-quality data involves several preprocessing techniques:
- Data cleaning: This involves identifying and correcting errors or inconsistencies in the data. Common issues include missing values, duplicates, and outliers. Rapid Innovation employs advanced AI algorithms to automate data cleaning processes, significantly reducing time and effort. This can include free raw dna analysis and raw dna health analysis.
- Normalization: This technique adjusts the data to bring different scales to a common scale, which is essential for accurate comparisons and analyses.
- Transformation: Data transformation techniques, such as log transformation or scaling, can help in stabilizing variance and making the data more suitable for analysis.
Implementing these preprocessing techniques can significantly enhance the reliability of the results obtained from data analysis. Additionally, employing robust data validation methods ensures that the data used in research is accurate and representative of the population being studied.
- Automated tools: Utilizing software tools for data preprocessing can streamline the process and reduce human error. Rapid Innovation offers tailored software solutions that integrate seamlessly into existing workflows, including tools for raw dna data interpretation and genetic data analysis.
- Continuous monitoring: Regularly assessing data quality throughout the research process helps in maintaining high standards.
3.3. Addressing Data Scarcity in Rare Conditions
Data scarcity is a significant challenge in studying rare conditions, where limited patient populations can hinder research efforts. Addressing this issue requires innovative strategies:
- Collaborative networks: Establishing collaborations among researchers, institutions, and patient advocacy groups can help pool resources and data. Initiatives like the Global Rare Disease Network facilitate data sharing and collaboration.
- Use of registries: Patient registries can collect and maintain data on individuals with rare conditions, providing a valuable resource for researchers.
- Leveraging technology: Advanced technologies, such as artificial intelligence and machine learning, can analyze small datasets effectively, identifying patterns that may not be apparent through traditional methods. Rapid Innovation specializes in developing AI models that can extract meaningful insights from limited data, enhancing research outcomes. This includes services like 3rd party dna analysis and raw genetic data analysis.
Additionally, researchers can utilize synthetic data generation techniques to create artificial datasets that mimic real-world data, allowing for more extensive testing of hypotheses and models.
- Crowdsourcing data: Engaging patients and families in data collection through mobile apps or online platforms can help gather more information about rare conditions.
- Focus on case studies: Detailed case studies of individual patients can provide insights into the condition, even when large datasets are unavailable. This can be complemented by raw data genetic analysis and gene sequence analysis.
By employing these strategies, researchers can overcome the challenges posed by data scarcity and advance the understanding of rare conditions, ultimately leading to better diagnosis and treatment options. Rapid Innovation is committed to supporting clients in these endeavors, ensuring they achieve greater ROI through effective use of AI technologies, including best raw dna data analysis and genetic network analysis. For more information on the importance of data quality in AI implementations.
3.4. Synthetic Data Generation for Training
Synthetic data generation is a crucial technique in the field of artificial intelligence (AI) and machine learning (ML). It involves creating artificial datasets that mimic real-world data without compromising privacy or security. This approach is particularly beneficial in scenarios where obtaining real data is challenging due to privacy concerns, data scarcity, or high costs.
- Enhances model training: Synthetic data can be used to train AI models effectively, allowing them to learn patterns and make predictions. It helps in overcoming the limitations of small datasets, which can lead to overfitting. At Rapid Innovation, we leverage synthetic data to ensure our clients' models are robust and capable of delivering high performance. This includes using synthetic training data and synthetic test data to validate model performance.
- Addresses privacy concerns: By generating synthetic data, organizations can avoid using sensitive personal information, thus adhering to privacy regulations like GDPR and HIPAA. This method ensures that the data used for training does not expose individuals' identities, allowing our clients to innovate without the fear of compliance issues. The use of synthetic data ai solutions further enhances this capability.
- Supports diverse scenarios: Synthetic data can be tailored to represent various scenarios, including rare events that may not be present in real datasets. This flexibility allows for more robust model training and better generalization in real-world applications, ultimately leading to greater ROI for our clients. For instance, synthetic data generation can be applied in synthetic image generation to create diverse visual datasets.
- Cost-effective: Generating synthetic data can be more economical than collecting and annotating real data, especially in specialized fields like healthcare or finance. Rapid Innovation helps clients reduce costs while maintaining high-quality data for their AI initiatives. The creation of synthetic datasets can significantly lower the financial burden associated with data acquisition.
- Tools and techniques: Various tools and frameworks, such as Generative Adversarial Networks (GANs) and Variational Autoencoders (VAEs), are commonly used for synthetic data generation. These technologies can produce high-quality data that closely resembles real-world distributions, enabling our clients to harness the power of AI effectively. Additionally, we provide guidance on synthetic data generation python libraries to facilitate this process. For more information on our services, visit our Enterprise AI Development page.
3.5. Privacy and Security Frameworks
Privacy and security frameworks are essential for ensuring that AI systems operate within ethical and legal boundaries. These frameworks provide guidelines and best practices for managing sensitive data, protecting user privacy, and securing AI systems against potential threats.
- Regulatory compliance: Organizations must comply with various regulations, such as GDPR, CCPA, and HIPAA, which dictate how personal data should be handled. Implementing a robust privacy framework helps organizations avoid legal penalties and build trust with users. Rapid Innovation assists clients in navigating these complex regulations to ensure compliance.
- Data protection measures: Encryption, anonymization, and pseudonymization are key techniques used to protect sensitive data. These measures ensure that even if data is compromised, it cannot be easily traced back to individuals, safeguarding our clients' reputations.
- Risk assessment: Regular risk assessments help identify vulnerabilities in AI systems and data handling processes. Organizations should conduct audits and penetration testing to evaluate their security posture. Rapid Innovation provides comprehensive risk assessment services to enhance our clients' security frameworks.
- User consent and transparency: Obtaining informed consent from users before collecting their data is a fundamental aspect of privacy frameworks. Transparency in data usage and processing helps build user trust and encourages responsible AI practices, which we prioritize in our consulting services.
- Incident response plans: Organizations should have clear incident response plans in place to address data breaches or security incidents. These plans should outline steps for containment, investigation, and communication with affected parties. Rapid Innovation helps clients develop and implement effective incident response strategies.
4. AI Diagnostic Agent Architecture
AI diagnostic agent architecture refers to the structural design of AI systems that are capable of diagnosing issues, providing insights, and making recommendations based on data analysis. This architecture is pivotal in various applications, including healthcare, IT support, and customer service.
- Modular design: A well-structured AI diagnostic agent typically consists of several modules, each responsible for specific tasks such as data collection, analysis, and reporting. This modularity allows for easier updates and maintenance, as individual components can be modified without affecting the entire system.
- Data integration: The architecture should support the integration of diverse data sources, including structured and unstructured data. This capability enables the agent to analyze comprehensive datasets, leading to more accurate diagnostics.
- Machine learning algorithms: AI diagnostic agents leverage machine learning algorithms to identify patterns and anomalies in data. These algorithms can be trained on historical data to improve their predictive capabilities over time.
- User interface: A user-friendly interface is essential for facilitating interaction between users and the AI diagnostic agent. The interface should provide clear visualizations and actionable insights, making it easier for users to understand the diagnostics.
- Feedback loop: Incorporating a feedback loop allows the AI diagnostic agent to learn from user interactions and improve its performance. Continuous learning enhances the agent's ability to provide relevant and timely recommendations.
- Scalability: The architecture should be designed to scale efficiently as data volume and complexity increase. This scalability ensures that the AI diagnostic agent remains effective in dynamic environments.
- Security considerations: Security measures must be integrated into the architecture to protect sensitive data and ensure compliance with privacy regulations. Regular updates and monitoring are necessary to safeguard against emerging threats. Rapid Innovation emphasizes the importance of security in the design and implementation of AI systems, ensuring our clients' solutions are both effective and secure.
4.1. System Design Principles
System design principles are foundational guidelines that help in creating effective and efficient systems. These principles ensure that the system is user-friendly, scalable, and maintainable. Key design principles include:
- Modularity: Breaking down the system into smaller, manageable components allows for easier updates and maintenance. Each module can be developed, tested, and deployed independently, which aligns with Rapid Innovation's approach to delivering tailored solutions that adapt to client needs.
- Scalability: The system should be designed to handle increasing amounts of data and users without performance degradation. This can be achieved through cloud-based solutions or distributed architectures, enabling clients to grow their operations without the need for extensive re-engineering.
- Usability: A user-centered design approach ensures that the system is intuitive and easy to navigate. This includes clear interfaces, helpful prompts, and accessible features for all users, ultimately enhancing user satisfaction and productivity.
- Interoperability: The system should be able to communicate and exchange data with other systems seamlessly. This is crucial in healthcare, where integration with electronic health records (EHR) and other medical systems is necessary. Rapid Innovation specializes in creating interoperable systems that facilitate smooth data exchange, leading to improved patient care.
- Security: Protecting sensitive patient data is paramount. Implementing robust security measures, such as encryption and access controls, helps safeguard against data breaches, ensuring compliance with industry regulations and building trust with users.
- Performance: The system should be optimized for speed and efficiency. This includes minimizing load times and ensuring quick response rates to user queries, which is essential for maintaining high levels of user engagement and operational efficiency.
- Maintainability: The design should facilitate easy updates and bug fixes. This can be achieved through clear documentation and adherence to coding standards, allowing Rapid Innovation to provide ongoing support and enhancements to clients' healthcare system design and medical system design.
4.2. Patient History Analysis Component

The Patient History Analysis Component is a critical part of any healthcare system, as it provides insights into a patient's medical background. This component helps healthcare providers make informed decisions based on comprehensive patient data. Key features include:
- Data Collection: Gathering detailed patient history, including past illnesses, surgeries, medications, and family history. This data can be collected through questionnaires or direct input from healthcare providers, ensuring a comprehensive understanding of patient needs.
- Data Integration: Combining patient history with other relevant data sources, such as lab results and imaging studies, to create a holistic view of the patient's health. Rapid Innovation excels in integrating diverse data sources to enhance clinical decision-making.
- Trend Analysis: Identifying patterns and trends in a patient's medical history can help predict future health issues. For example, recognizing recurring symptoms or conditions can lead to proactive management, ultimately improving patient outcomes.
- Risk Assessment: Utilizing algorithms to assess the risk of developing certain conditions based on the patient's history. This can guide preventive measures and early interventions, allowing healthcare providers to allocate resources more effectively.
- User Interface: Providing healthcare professionals with an intuitive interface to easily access and analyze patient history. This includes visualizations and summaries that highlight key information, streamlining workflows and enhancing user experience.
- Compliance and Standards: Ensuring that the component adheres to healthcare regulations and standards, such as HIPAA, to protect patient privacy and data security. Rapid Innovation prioritizes compliance, helping clients navigate complex regulatory environments.
4.3. Symptom Pattern Recognition Module
The Symptom Pattern Recognition Module is designed to analyze and identify patterns in patient symptoms, aiding in diagnosis and treatment planning. This module leverages advanced technologies to enhance clinical decision-making. Key aspects include:
- Data Input: Collecting symptom data from patients through surveys, mobile apps, or direct input during consultations. This data should be structured for easy analysis, enabling healthcare providers to make informed decisions quickly.
- Machine Learning Algorithms: Implementing machine learning techniques to recognize patterns in symptom data. These algorithms can learn from historical data to improve accuracy over time, ensuring that healthcare providers have access to the most relevant insights.
- Symptom Correlation: Identifying correlations between different symptoms and potential diagnoses. This can help healthcare providers narrow down possible conditions based on the symptoms presented, ultimately leading to more accurate diagnoses.
- Real-time Analysis: Providing real-time analysis of symptoms as they are reported, allowing for immediate feedback and recommendations for further action. This capability enhances the responsiveness of healthcare providers to patient needs.
- Decision Support: Offering decision support tools that suggest possible diagnoses or next steps based on the recognized symptom patterns. This can enhance the efficiency of clinical workflows, allowing healthcare professionals to focus on patient care.
- Continuous Learning: The module should be designed to continuously learn from new data, improving its predictive capabilities and adapting to emerging health trends. Rapid Innovation's commitment to continuous improvement ensures that clients benefit from the latest advancements in AI technology.
- User Feedback: Incorporating feedback from healthcare professionals to refine the module's algorithms and improve its usability and effectiveness in clinical settings. This collaborative approach ensures that the solutions provided by Rapid Innovation are aligned with the real-world needs of healthcare providers.
4.4. Biomarker Identification Subsystem
The Biomarker Identification Subsystem is a critical component in the realm of personalized medicine and diagnostics. This subsystem focuses on identifying biological markers that can indicate the presence or progression of a disease.
- Utilizes advanced algorithms and machine learning techniques to analyze large datasets, including large scale microbiome data integration enables robust biomarker identification.
- Integrates genomic, proteomic, and metabolomic data to identify potential biomarkers through various biomarker identification techniques.
- Aims to enhance early detection of diseases, leading to better patient outcomes.
- Supports the development of targeted therapies by identifying specific biomarkers associated with certain conditions.
- Collaborates with clinical data to validate the clinical relevance of identified biomarkers.
The importance of this subsystem lies in its ability to provide insights that can lead to more accurate diagnoses and tailored treatment plans. By identifying biomarkers, healthcare professionals can make informed decisions that improve patient care, ultimately driving greater ROI for healthcare organizations through enhanced treatment efficacy and reduced costs associated with late-stage disease management. For more information on how advanced technologies can aid in this process, check out our AI agents for patient care.
4.5. Genetic Variant Analysis Engine
The Genetic Variant Analysis Engine is designed to analyze genetic variations within an individual's genome. This engine plays a pivotal role in understanding how genetic differences can influence health and disease.
- Employs bioinformatics tools to assess single nucleotide polymorphisms (SNPs) and other genetic variants.
- Facilitates the identification of variants that may contribute to disease susceptibility or drug response.
- Integrates data from various genomic databases to provide comprehensive variant annotations.
- Supports clinical decision-making by predicting the potential impact of genetic variants on patient health.
- Enhances research capabilities by enabling the exploration of genotype-phenotype relationships.
This engine is essential for precision medicine, as it allows for the customization of treatment based on an individual's genetic makeup. By understanding genetic variants, healthcare providers can offer more effective and personalized care, leading to improved patient outcomes and increased operational efficiency, thereby maximizing ROI for healthcare institutions.
4.6. Diagnostic Reasoning and Inference System
The Diagnostic Reasoning and Inference System is a sophisticated tool that aids healthcare professionals in making accurate diagnoses. This system leverages artificial intelligence and clinical knowledge to support clinical reasoning.
- Analyzes patient data, including symptoms, medical history, and test results, to generate differential diagnoses.
- Utilizes rule-based algorithms and machine learning to improve diagnostic accuracy over time.
- Provides evidence-based recommendations for further testing or treatment options.
- Enhances clinical workflows by streamlining the diagnostic process and reducing time to diagnosis.
- Supports continuous learning by incorporating new medical knowledge and guidelines into its reasoning framework.
The significance of this system lies in its ability to reduce diagnostic errors and improve patient safety. By providing healthcare professionals with reliable diagnostic support, it enhances the overall quality of care delivered to patients, which not only fosters trust but also contributes to better financial performance for healthcare providers through reduced liability and improved patient retention.
4.7. Uncertainty Quantification Mechanisms
Uncertainty quantification (UQ) mechanisms are essential in various fields, particularly in healthcare and clinical research. These mechanisms help in assessing the reliability and accuracy of models and predictions, which is crucial for making informed decisions.
- Definition: UQ refers to the process of quantifying uncertainties in both computational and experimental models. It involves identifying, characterizing, and reducing uncertainties to improve the robustness of predictions.
- Importance in Healthcare:
- Enhances decision-making by providing a clearer understanding of potential risks and outcomes.
- Supports the development of personalized medicine by accounting for variability in patient responses.
- Facilitates regulatory compliance by ensuring that models meet required standards of reliability.
- Common UQ Techniques:
- Sensitivity Analysis: Identifies how variations in input parameters affect model outputs.
- Monte Carlo Simulations: Uses random sampling to estimate the probability distribution of outcomes.
- Bayesian Methods: Incorporates prior knowledge and evidence to update the probability of outcomes.
- Applications in Clinical Settings:
- Risk assessment in treatment plans, helping clinicians understand the likelihood of adverse events.
- Predictive modeling for disease progression, allowing for tailored interventions.
- Evaluation of diagnostic tools, ensuring their accuracy and reliability in diverse populations.
- Challenges:
- Complexity of biological systems makes it difficult to quantify uncertainties accurately.
- Limited data availability can hinder effective UQ.
- Need for interdisciplinary collaboration to integrate UQ into clinical workflows.
5. Clinical Integration Framework
A clinical integration framework is a structured approach that facilitates the seamless incorporation of technology, particularly artificial intelligence (AI), into healthcare practices. This framework aims to enhance patient care, improve outcomes, and streamline workflows.
- Key Components:
- Interoperability: Ensures that different systems and technologies can communicate and share data effectively.
- Standardization: Establishes common protocols and guidelines for data collection, analysis, and reporting.
- Stakeholder Engagement: Involves healthcare professionals, patients, and technology developers in the integration process.
- Benefits:
- Improved patient outcomes through data-driven decision-making.
- Enhanced efficiency in clinical workflows, reducing administrative burdens on healthcare providers.
- Better resource allocation by identifying areas for improvement and optimization.
- Implementation Strategies:
- Pilot Programs: Test the integration of AI tools in specific departments before a full-scale rollout.
- Training and Education: Provide healthcare professionals with the necessary skills to utilize AI effectively.
- Continuous Evaluation: Regularly assess the impact of integrated technologies on patient care and operational efficiency.
5.1. Physician-AI Collaborative Workflow
The physician-AI collaborative workflow is a model that emphasizes the partnership between healthcare professionals and AI systems. This collaboration aims to enhance clinical decision-making and improve patient care.
- Workflow Characteristics:
- Complementarity: AI systems assist physicians by providing insights and recommendations, rather than replacing human judgment.
- Real-time Data Analysis: AI tools analyze patient data quickly, offering timely support for clinical decisions.
- Feedback Loop: Physicians can provide feedback on AI recommendations, allowing for continuous improvement of the algorithms.
- Advantages:
- Increased diagnostic accuracy through AI's ability to process vast amounts of data.
- Reduced cognitive load on physicians, enabling them to focus on patient interaction and care.
- Enhanced patient engagement by providing personalized treatment options based on AI analysis.
- Challenges:
- Trust and Acceptance: Physicians may be hesitant to rely on AI due to concerns about accuracy and accountability.
- Data Privacy: Ensuring patient data is protected while using AI tools is critical.
- Integration with Existing Systems: Seamless incorporation of AI into current workflows can be complex and resource-intensive.
- Future Directions:
- Development of user-friendly AI interfaces that facilitate easy interaction for physicians.
- Ongoing research to improve AI algorithms, ensuring they are trained on diverse datasets for better generalization.
- Establishing guidelines for ethical AI use in clinical settings, addressing concerns about bias and transparency.
At Rapid Innovation, we leverage our expertise in AI to implement these uncertainty quantification in healthcare mechanisms and clinical integration frameworks, helping our clients achieve greater ROI through improved decision-making, enhanced patient outcomes, and streamlined workflows. By collaborating with healthcare professionals, we ensure that our AI solutions are tailored to meet the specific needs of the industry, ultimately driving efficiency and effectiveness in clinical settings. For more information on our services, visit our AI consulting company.
5.2. User Interface Design for Clinical Settings

User interface (UI) design in clinical settings is crucial for enhancing the efficiency and effectiveness of healthcare delivery. A well-designed UI can significantly improve user experience for healthcare professionals and patients alike.
- Clarity and Simplicity: The interface should be intuitive, allowing users to navigate easily without extensive training. Clear labeling and straightforward workflows are essential.
- Accessibility: Design must accommodate users with varying levels of tech-savviness and physical abilities. This includes using larger fonts, high-contrast colors, and voice commands.
- Consistency: Consistent design elements across different screens help users predict outcomes and reduce cognitive load. This includes uniform button styles, color schemes, and iconography.
- Feedback Mechanisms: Providing immediate feedback for user actions (e.g., confirmations, error messages) helps users understand the system's responses and reduces frustration.
- Customization: Allowing users to customize their dashboards or interfaces can enhance usability. Healthcare professionals often have different needs based on their specialties.
- Integration with Clinical Workflows: The UI should seamlessly integrate with existing clinical workflows to minimize disruptions. This includes easy access to patient records, lab results, and treatment protocols.
At Rapid Innovation, we specialize in developing tailored UI solutions that address these critical aspects, ensuring that healthcare organizations can enhance their operational efficiency and improve user satisfaction. Our expertise in AI-driven design allows us to create interfaces that not only meet the current needs of healthcare providers but also adapt to future requirements, ultimately leading to greater ROI. Additionally, we offer services such as chatbot development to further enhance user interaction and support in clinical environments. We also explore the use of AI agents for patient support to improve patient engagement and care delivery.
5.3. Decision Support Implementation
Decision support systems (DSS), including clinical decision support systems (CDSS), are vital in clinical settings, aiding healthcare professionals in making informed decisions. Effective implementation of these systems can lead to improved patient outcomes and operational efficiency.
- Evidence-Based Guidelines: Incorporating clinical guidelines and protocols into the CDSS ensures that healthcare providers have access to the latest evidence-based practices.
- Real-Time Data Access: Decision support tools should provide real-time access to patient data, lab results, and medical history, enabling timely and informed decision-making.
- User-Friendly Interfaces: The design of clinical decision support tools should prioritize usability, ensuring that healthcare professionals can easily interpret and act on the information provided.
- Integration with EHR Systems: Seamless integration with electronic health records (EHR) is essential for a comprehensive view of patient data, allowing for more accurate decision-making.
- Training and Support: Providing adequate training and ongoing support for healthcare professionals is crucial for successful implementation. This helps users feel confident in utilizing the system effectively.
- Feedback and Iteration: Continuous feedback from users can help refine and improve the clinical decision support system over time, ensuring it meets the evolving needs of healthcare providers.
Rapid Innovation's expertise in AI allows us to implement advanced decision support systems that enhance clinical decision-making processes. By leveraging real-time data and evidence-based guidelines, we empower healthcare professionals to make informed choices that lead to better patient outcomes and increased operational efficiency.
5.4. Alert and Notification Systems
Alert and notification systems play a critical role in clinical settings by ensuring timely communication of important information. These systems can enhance patient safety and improve clinical outcomes.
- Timeliness: Alerts must be delivered promptly to ensure that healthcare providers can respond quickly to critical situations, such as abnormal lab results or medication interactions.
- Relevance: Notifications should be tailored to the specific needs of the user, reducing alert fatigue. This means prioritizing alerts based on severity and relevance to the patient's condition.
- Clear Messaging: Alerts should be concise and clear, providing essential information without overwhelming the user. This includes specifying the nature of the alert and recommended actions.
- Escalation Protocols: Implementing escalation protocols for alerts ensures that critical notifications are addressed promptly. This may involve notifying multiple team members if an alert is not acknowledged.
- Integration with Clinical Workflows: Alerts should be integrated into existing clinical workflows to ensure that they are actionable and do not disrupt the provider's routine.
- User Preferences: Allowing users to customize their alert settings can enhance the effectiveness of the system. This includes options for how and when to receive notifications.
By focusing on these aspects, healthcare organizations can create user-friendly interfaces, implement effective clinical decision support systems, and establish robust alert and notification systems that enhance patient care and operational efficiency. Rapid Innovation is committed to delivering innovative solutions that not only meet the immediate needs of healthcare providers but also drive long-term value and ROI through enhanced patient safety and improved clinical outcomes.
5.5. Documentation and Reporting Standards
Documentation and reporting standards are essential components in any project, particularly in fields like data science, software development, and research. These standards ensure that all stakeholders have access to clear, consistent, and comprehensive information regarding the project’s progress, methodologies, and outcomes.
- Clarity and Consistency: Documentation should be clear and consistent across all platforms. This includes using standardized terminology and formats to avoid confusion. For example, adhering to financial reporting standards such as GAAP required financial statements can enhance clarity.
- Comprehensive Reporting: Reports should cover all aspects of the project, including objectives, methodologies, results, and conclusions. This ensures that anyone reviewing the documentation can understand the project’s scope and findings. Incorporating elements like XBRL reports can provide structured financial data.
- Version Control: Implementing version control for documentation helps track changes over time. This is crucial for maintaining the integrity of the information and for auditing purposes, especially in compliance with standards like SOC 1 compliance checklist.
- Accessibility: Documentation should be easily accessible to all relevant stakeholders. This can be achieved through centralized repositories or cloud-based platforms, ensuring that resources like IFRS standards PDF and ISO audit schedule are readily available.
- Compliance: Adhering to industry-specific documentation standards (such as ISO, IEEE, or specific regulatory requirements) is vital for ensuring that the project meets legal and ethical guidelines. For instance, compliance with IFRS sustainability standards is increasingly important.
- Visual Aids: Incorporating charts, graphs, and other visual aids can enhance understanding and retention of information. Visuals can help convey complex data in a more digestible format, which is particularly useful when summarizing concepts like ASC 606 summary or GASB 34 summary.
- Regular Updates: Documentation should be updated regularly to reflect any changes in the project. This includes updates on methodologies, results, and any challenges faced during the project lifecycle, such as those encountered in audit procedures for leases IFRS 16.
6. Training and Validation Methodologies
Training and validation methodologies are critical in ensuring the effectiveness and reliability of models in machine learning and data science. These methodologies help in assessing how well a model performs and its ability to generalize to unseen data.
- Importance of Training: Training involves teaching a model to recognize patterns in data. This is done using a training dataset, which is a subset of the overall data, similar to how financial data is prepared for analysis in XBRL financial statements.
- Validation Techniques: Validation methodologies help in evaluating the model’s performance. Common techniques include:
- Cross-Validation: This involves dividing the dataset into multiple subsets and training the model on different combinations of these subsets to ensure robustness.
- Holdout Method: This method splits the dataset into training and testing sets, allowing for a straightforward evaluation of the model’s performance on unseen data.
- Hyperparameter Tuning: This process involves adjusting the parameters of the model to improve its performance. Techniques such as grid search or random search can be employed to find the optimal settings.
- Performance Metrics: Various metrics are used to evaluate model performance, including accuracy, precision, recall, and F1 score. Choosing the right metric is crucial depending on the specific application and goals of the model, such as those outlined in the FASB conceptual framework PDF.
- Continuous Learning: Incorporating feedback loops and continuous learning mechanisms can help improve model performance over time. This involves retraining the model with new data as it becomes available, similar to how organizations might update their internal audit schedule template ISO 9001 2015.
6.1. Supervised Learning Approaches
Supervised learning is a type of machine learning where models are trained on labeled datasets. This means that the input data is paired with the correct output, allowing the model to learn the relationship between the two.
- Definition: In supervised learning, the algorithm learns from a training dataset that includes both input features and the corresponding output labels.
- Types of Supervised Learning:
- Classification: This approach is used when the output variable is categorical. For example, classifying emails as spam or not spam.
- Regression: This approach is used when the output variable is continuous. For instance, predicting house prices based on various features.
- Algorithms Used:
- Decision Trees: These models use a tree-like structure to make decisions based on input features.
- Support Vector Machines (SVM): SVMs are effective for high-dimensional spaces and are used for both classification and regression tasks.
- Neural Networks: These models are inspired by the human brain and are particularly effective for complex tasks such as image and speech recognition.
- Training Process: The training process involves feeding the model with labeled data, allowing it to learn the mapping from inputs to outputs. The model is then validated using a separate dataset to assess its performance.
- Challenges:
- Overfitting: This occurs when a model learns the training data too well, including noise and outliers, leading to poor performance on new data.
- Data Quality: The quality of the labeled data is crucial. Poor quality data can lead to inaccurate models.
- Applications: Supervised learning is widely used in various fields, including finance for credit scoring, healthcare for disease diagnosis, and marketing for customer segmentation. For example, the application of IFRS 17 summary PDF can be crucial in financial modeling.
By adhering to documentation and reporting standards, employing effective training and validation methodologies, and utilizing supervised learning approaches, organizations can enhance their data-driven decision-making processes and improve overall project outcomes. At Rapid Innovation, we leverage these methodologies to help our clients achieve greater ROI by ensuring that their AI projects are well-documented, effectively trained, and validated, leading to more reliable and actionable insights. For more insights on the importance of data annotation services.
6.2. Few-Shot and Zero-Shot Learning Techniques

Few-shot and zero-shot learning techniques are gaining traction in the field of machine learning, particularly in applications like medical diagnostics. These methods allow models to make predictions with limited labeled data, which is often a challenge in healthcare due to the scarcity of annotated datasets.
- Few-shot learning involves training a model on a small number of examples from each class. This is particularly useful in scenarios where collecting large datasets is impractical, enabling healthcare providers to quickly adapt to new conditions without extensive data collection.
- Zero-shot learning, on the other hand, enables models to recognize classes they have never seen before by leveraging semantic information. For instance, a model trained on images of cats and dogs can identify a horse if it understands the concept of "four-legged animals." This capability can be transformative in healthcare, allowing for the identification of new diseases based on existing knowledge.
- These techniques can significantly reduce the time and cost associated with data collection and labeling, making them ideal for rare diseases or conditions with limited case studies. Rapid Innovation can assist clients in implementing these few-shot learning healthcare techniques to enhance their diagnostic capabilities while minimizing resource expenditure.
- Applications in healthcare include identifying rare diseases from medical images or predicting patient outcomes based on minimal historical data. By leveraging Rapid Innovation's expertise, clients can achieve greater ROI through improved diagnostic accuracy and faster time-to-market for new healthcare solutions. For more information on how Rapid Innovation can help with large language model development, visit large language model development.
6.3. Transfer Learning from Common Diseases
Transfer learning is a powerful technique that allows models trained on one task to be adapted for another, often related, task. In the context of healthcare, this means leveraging knowledge gained from common diseases to improve the diagnosis and treatment of less common conditions.
- By using pre-trained models on large datasets of common diseases, healthcare practitioners can save time and resources when developing models for rare diseases. Rapid Innovation can guide clients in selecting and fine-tuning these models to maximize their effectiveness.
- Transfer learning can enhance model performance by providing a strong starting point, especially when the new dataset is small or lacks diversity. This approach not only accelerates development but also leads to more reliable outcomes.
- This approach is particularly beneficial in medical imaging, where models trained on large datasets like ImageNet can be fine-tuned for specific medical applications, such as detecting tumors in MRI scans. Rapid Innovation's expertise in this area ensures that clients can leverage the latest advancements in AI to improve patient care.
- The ability to transfer knowledge from common to rare diseases can lead to improved diagnostic accuracy and better patient outcomes. By partnering with Rapid Innovation, clients can harness this potential to drive innovation in their healthcare offerings.
6.4. Reinforcement Learning for Diagnostic Pathways
Reinforcement learning (RL) is an area of machine learning where agents learn to make decisions by interacting with an environment. In healthcare, RL can be applied to optimize diagnostic pathways, leading to more efficient and effective patient care.
- RL algorithms can be used to model the decision-making process in diagnostics, where the agent learns from the outcomes of its actions. Rapid Innovation can help clients implement RL solutions that adapt to real-world clinical environments.
- By simulating various diagnostic pathways, RL can identify the most effective sequences of tests and treatments, reducing unnecessary procedures and improving patient outcomes. This capability can lead to significant cost savings and enhanced patient satisfaction.
- This technique can adapt to individual patient data, allowing for personalized treatment plans based on real-time feedback. Rapid Innovation's expertise in AI can empower clients to create tailored healthcare solutions that meet the unique needs of their patient populations.
- RL has the potential to streamline clinical workflows, reduce costs, and enhance the overall quality of care by ensuring that patients receive the most appropriate diagnostics and treatments based on their unique conditions. By collaborating with Rapid Innovation, clients can unlock the full potential of AI in their healthcare practices, driving efficiency and improving patient outcomes.
6.5. Validation Strategies for Rare Conditions
Validating diagnostic tests for rare conditions presents unique challenges due to the limited availability of patient populations and data. Effective validation strategies are essential to ensure the reliability and accuracy of these tests.
- Use of Reference Standards: Establishing a gold standard for diagnosis is crucial. This may involve using established clinical criteria or consensus guidelines to validate new tests.
- Retrospective Studies: Analyzing existing patient data can provide insights into the test's performance. This approach allows researchers to assess the test's accuracy without needing a large number of new patients.
- Multi-Center Collaborations: Partnering with multiple healthcare institutions can increase the sample size and diversity of the patient population. This collaboration enhances the robustness of validation studies.
- Patient Registries: Utilizing patient registries can help gather data on rare conditions. These registries often contain valuable information that can be used to validate diagnostic tests.
- Adaptive Trial Designs: Implementing adaptive designs allows for modifications to the study based on interim results. This flexibility can be particularly beneficial in rare conditions where patient recruitment is challenging.
- Statistical Methods: Employing advanced statistical techniques, such as Bayesian methods, can help in interpreting data from small sample sizes. These methods can provide more reliable estimates of test performance. For more information on how AI can assist in these validation strategies, visit our article on AI Agents in Software Testing.
6.6. Performance Metrics and Evaluation Criteria
Performance metrics and evaluation criteria are vital for assessing the effectiveness of diagnostic tests. These metrics help determine how well a test performs in identifying a condition.
- Sensitivity and Specificity: Sensitivity measures the test's ability to correctly identify those with the condition (true positive rate), while specificity measures the test's ability to correctly identify those without the condition (true negative rate).
- Positive Predictive Value (PPV) and Negative Predictive Value (NPV): PPV indicates the probability that subjects with a positive test truly have the condition, whereas NPV indicates the probability that subjects with a negative test truly do not have the condition.
- Accuracy: This metric reflects the overall correctness of the test, calculated as the proportion of true results (both true positives and true negatives) among the total number of cases examined.
- Area Under the Receiver Operating Characteristic Curve (AUC-ROC): This metric evaluates the test's ability to discriminate between those with and without the condition. A higher AUC indicates better performance.
- Likelihood Ratios: These ratios help assess how much a test result will change the odds of having a condition. They are useful for interpreting test results in clinical practice.
- Clinical Utility: Beyond statistical performance, evaluating how the test impacts patient management and outcomes is crucial. This includes assessing whether the test leads to better treatment decisions and improved patient outcomes.
7. Specialized Diagnostic Capabilities
Specialized diagnostic capabilities are essential for accurately identifying and managing complex or rare conditions. These capabilities often involve advanced technologies and methodologies.
- Genetic Testing: Genetic tests can identify mutations associated with rare diseases, providing critical information for diagnosis and treatment. Next-generation sequencing (NGS) allows for comprehensive analysis of genetic material, enabling the detection of multiple conditions simultaneously.
- Biomarker Discovery: Identifying specific biomarkers can enhance diagnostic accuracy. Biomarkers can be proteins, genes, or other molecules that indicate the presence of a disease.
- Imaging Techniques: Advanced imaging modalities, such as MRI, PET scans, and CT scans, can provide detailed insights into the physiological changes associated with rare conditions.
- Artificial Intelligence (AI) and Machine Learning: AI algorithms can analyze complex datasets to identify patterns that may not be apparent to human clinicians. Machine learning models can improve diagnostic accuracy by learning from large datasets and continuously refining their predictions. At Rapid Innovation, we leverage AI to enhance diagnostic capabilities, ensuring that our clients can achieve greater ROI through improved accuracy and efficiency in their diagnostic processes.
- Point-of-Care Testing: Rapid diagnostic tests that can be performed at the point of care improve access to testing for rare conditions, facilitating timely diagnosis and treatment.
- Telemedicine and Remote Monitoring: These technologies enable specialists to consult with patients in remote areas, expanding access to specialized diagnostic capabilities and improving patient outcomes.
- Interdisciplinary Collaboration: Collaboration among specialists from various fields can enhance diagnostic capabilities. This approach ensures that all aspects of a rare condition are considered, leading to more accurate diagnoses and better patient care. Rapid Innovation fosters such collaborations, helping clients integrate diverse expertise to optimize their diagnostic strategies.
7.1. Pediatric Rare Disease Detection
Pediatric rare disease detection is crucial for early diagnosis and intervention, which can significantly improve outcomes for affected children. Rare diseases are defined as conditions that affect fewer than 200,000 individuals in the United States.
- Early detection can lead to timely treatment, which is essential for managing symptoms and improving quality of life. Rapid Innovation leverages AI-driven analytics to enhance early detection capabilities, enabling healthcare providers to identify potential rare diseases more efficiently.
- Advances in genetic testing and screening technologies have made it easier to identify rare diseases in children. Our AI solutions can analyze genetic data at scale, providing insights that facilitate quicker diagnoses.
- Newborn screening programs are increasingly incorporating tests for rare genetic disorders, allowing for early intervention. Rapid Innovation collaborates with healthcare organizations to integrate AI tools that streamline the screening process and improve accuracy.
- Telemedicine and digital health tools are enhancing access to specialists who can diagnose and manage rare pediatric conditions. Our AI-powered platforms support remote consultations, ensuring that families receive timely expert advice regardless of location.
- Collaboration among healthcare providers, researchers, and families is vital for sharing information and resources related to rare diseases. Rapid Innovation fosters these collaborations through data-sharing platforms that utilize AI to connect stakeholders effectively. For more information on how we can assist, visit our healthcare chatbot development and AI technology consulting services.
7.2. Genetic and Metabolic Disorders

Genetic and metabolic disorders encompass a wide range of conditions that arise from abnormalities in genes or metabolic processes. These disorders can have profound effects on a child's development and overall health.
- Genetic disorders can be inherited or occur spontaneously due to mutations. Examples include cystic fibrosis, sickle cell disease, and Duchenne muscular dystrophy. Rapid Innovation's AI models can predict the likelihood of these disorders based on genetic profiles, aiding in proactive management.
- Metabolic disorders often result from enzyme deficiencies that disrupt normal biochemical processes. Conditions like phenylketonuria (PKU) and galactosemia fall into this category. Our AI solutions assist in analyzing metabolic data to identify potential disorders early.
- Early diagnosis through genetic testing can help manage these disorders effectively, often through dietary modifications or enzyme replacement therapies. Rapid Innovation provides AI-driven decision support tools that guide healthcare providers in creating personalized treatment plans.
- Advances in gene therapy are showing promise for treating certain genetic disorders, potentially correcting the underlying genetic defects. Our research initiatives focus on utilizing AI to optimize gene therapy approaches and improve patient outcomes.
- Ongoing research is essential to understand the complexities of these disorders and develop new treatment options. Rapid Innovation partners with research institutions to harness AI for data analysis, accelerating the discovery of innovative therapies.
7.3. Rare Autoimmune Conditions
Rare autoimmune conditions occur when the immune system mistakenly attacks the body's own tissues. These conditions can be challenging to diagnose and manage due to their rarity and the variability of symptoms.
- Examples of rare autoimmune diseases include systemic lupus erythematosus, scleroderma, and myositis. Rapid Innovation's AI algorithms can analyze patient data to identify patterns that may indicate these conditions, facilitating earlier diagnosis.
- Symptoms can vary widely, making it difficult for healthcare providers to identify these conditions promptly. Our AI solutions enhance diagnostic accuracy by integrating diverse data sources, providing a comprehensive view of patient health.
- Multidisciplinary approaches are often necessary for effective management, involving rheumatologists, immunologists, and other specialists. Rapid Innovation supports these approaches by developing collaborative platforms that enable seamless communication among healthcare teams.
- Research into the genetic and environmental factors contributing to these diseases is ongoing, with the goal of improving diagnosis and treatment. Our AI-driven research tools assist in identifying correlations and trends that can inform future studies.
- Patient advocacy groups play a crucial role in raising awareness and funding research for rare autoimmune conditions, helping to connect patients with resources and support. Rapid Innovation actively engages with these groups to ensure that our AI solutions align with patient needs and enhance their support networks.
7.4. Rare Neurological Disorders
Rare neurological disorders are conditions that affect the nervous system and occur infrequently in the general population. These disorders can significantly impact an individual's quality of life and often require specialized care.
- Examples of rare neurological disorders include:
- Huntington's Disease: A genetic disorder that causes the progressive breakdown of nerve cells in the brain.
- Amyotrophic Lateral Sclerosis (ALS): A progressive neurodegenerative disease that affects nerve cells in the brain and spinal cord.
- Wilson's Disease: A genetic disorder that leads to excessive copper accumulation in the body, affecting the liver and brain.
- Symptoms can vary widely but may include:
- Cognitive decline
- Motor dysfunction
- Seizures
- Behavioral changes
- Diagnosis often involves:
- Neurological examinations
- Genetic testing
- Imaging studies like MRI or CT scans
- Treatment options may include:
- Medications to manage symptoms
- Physical therapy
- Supportive care to improve quality of life
Due to their rarity, these disorders often face challenges in research funding and awareness, making it crucial for healthcare professionals to stay informed about the latest developments in diagnosis and treatment. At Rapid Innovation, we leverage AI-driven analytics to assist healthcare providers in identifying patterns and trends in rare neurological disorders, ultimately enhancing diagnostic accuracy and treatment efficacy.
7.5. Rare Oncological Conditions
Rare oncological conditions refer to uncommon types of cancer that affect a small percentage of the population. These cancers can be particularly challenging to diagnose and treat due to their rarity and the limited research available.
- Examples of rare oncological conditions include:
- Sarcomas: Cancers that arise from connective tissues, such as bone, muscle, and fat.
- Neuroendocrine Tumors: Tumors that develop from hormone-producing cells in the neuroendocrine system.
- Germ Cell Tumors: Tumors that originate from germ cells, which can develop into various types of cancer.
- Key characteristics of rare cancers:
- Often have unique symptoms that may be mistaken for more common conditions.
- May require specialized treatment approaches, including targeted therapies and clinical trials.
- Diagnosis typically involves:
- Imaging tests (CT, MRI, PET scans)
- Biopsies to confirm the presence of cancer cells
- Genetic testing to identify specific mutations
- Treatment options can include:
- Surgery to remove tumors
- Chemotherapy and radiation therapy
- Emerging therapies like immunotherapy and personalized medicine
Awareness and research into rare oncological conditions are essential for improving patient outcomes and developing new treatment strategies. Rapid Innovation employs machine learning algorithms to analyze vast datasets, enabling oncologists to identify potential treatment pathways and improve patient care, thereby maximizing return on investment in healthcare resources.
7.6. Rare Infectious Diseases
Rare infectious diseases are illnesses caused by pathogens that occur infrequently in the population. These diseases can pose significant public health challenges due to their unpredictability and the potential for outbreaks.
- Examples of rare infectious diseases include:
- Ebola Virus Disease: A severe illness caused by the Ebola virus, characterized by fever, vomiting, and bleeding.
- Nipah Virus Infection: A zoonotic disease that can cause severe respiratory illness and encephalitis.
- Hantavirus Pulmonary Syndrome: A severe respiratory disease caused by hantaviruses, often transmitted through rodent droppings.
- Common features of rare infectious diseases:
- Often have complex transmission routes, including zoonotic origins.
- Symptoms can range from mild to severe, depending on the pathogen and individual health.
- Diagnosis usually involves:
- Laboratory tests to identify the specific pathogen
- Serological tests to detect antibodies
- Clinical evaluation of symptoms and exposure history
- Treatment options may include:
- Antiviral medications for specific infections
- Supportive care to manage symptoms
- Vaccination in some cases, such as for Ebola
Public health initiatives and research are critical for understanding and controlling rare infectious diseases, especially in the context of global travel and climate change, which can influence the spread of these pathogens. Rapid Innovation's AI solutions can enhance surveillance systems, enabling quicker responses to outbreaks and more effective allocation of healthcare resources, ultimately leading to improved public health outcomes.
8. Explainable AI in Diagnostic Processes
Explainable AI (XAI) is becoming increasingly important in the field of healthcare, particularly in diagnostic processes. As AI systems are integrated into clinical settings, understanding how these systems arrive at their conclusions is crucial for trust, accountability, and effective patient care. The need for explainable AI in healthcare is underscored by the fact that AI in medicine must be explainable to ensure safe and effective patient care.
8.1 Transparency in Diagnostic Reasoning

Transparency in diagnostic reasoning refers to the ability of AI systems to provide clear and understandable explanations for their decisions. This is essential for several reasons:
- Trust Building: Clinicians and patients need to trust AI systems. When AI can explain its reasoning, it fosters confidence in its recommendations.
- Clinical Validation: Healthcare professionals can validate AI-generated diagnoses against their own knowledge and experience, which is particularly important in complex cases where human intuition plays a significant role.
- Regulatory Compliance: Many regulatory bodies are beginning to require transparency in AI systems. Clear reasoning can help meet these standards and ensure that AI tools are safe and effective.
- Error Identification: Understanding the reasoning behind AI decisions allows healthcare providers to identify potential errors or biases in the system, leading to improved outcomes.
- Patient Engagement: When patients understand the reasoning behind a diagnosis, they are more likely to engage in their treatment plans and adhere to medical advice.
To achieve transparency, AI systems can utilize various techniques, such as rule-based systems, decision trees, or model-agnostic methods that explain predictions in human-understandable terms. This aligns with the broader goal of explainable AI in healthcare and medicine.
8.2 Feature Importance Visualization
Feature importance visualization is a technique used to illustrate which factors or features most significantly influence the AI's diagnostic decisions. This is crucial for several reasons:
- Understanding Influences: By visualizing feature importance, clinicians can see which variables (e.g., symptoms, lab results, patient history) are driving the AI's conclusions, helping them understand the context of the diagnosis.
- Improving Model Performance: Identifying important features can guide data collection and model refinement. If certain features are consistently highlighted, it may indicate areas where more data is needed or where the model can be improved.
- Facilitating Collaboration: Visualizations can serve as a communication tool between AI systems and healthcare professionals, bridging the gap between technical AI experts and clinical practitioners.
- Enhancing Education: Feature importance visualizations can be used in training programs for healthcare professionals, helping them understand how AI systems work and how to interpret their outputs.
- Patient Communication: Visual aids can also be used to explain diagnoses to patients, making complex information more accessible and understandable.
Common methods for feature importance visualization include bar charts, heat maps, and SHAP (SHapley Additive exPlanations) values, which provide insights into how each feature contributes to the model's predictions. This is particularly relevant for explainable artificial intelligence for medical applications.
In conclusion, explainable AI in diagnostic processes is essential for fostering trust, improving clinical outcomes, and ensuring that AI systems are used effectively and ethically in healthcare settings. By focusing on transparency in diagnostic reasoning and utilizing feature importance visualization, healthcare professionals can better integrate explainable AI in healthcare into their practices, ultimately benefiting patient care.
At Rapid Innovation, we specialize in developing and implementing XAI solutions tailored to the healthcare sector. Our expertise ensures that your AI systems not only deliver accurate diagnoses but also provide the transparency needed to build trust among clinicians and patients alike. By leveraging our services, healthcare organizations can enhance their operational efficiency, improve patient outcomes, and achieve a greater return on investment.
8.3. Decision Path Explanation Methods
Decision path explanation methods are essential in understanding how machine learning models arrive at their conclusions. These methods provide insights into the decision-making process of algorithms, particularly in complex models like deep learning.
- Transparency: These methods enhance transparency by illustrating the steps taken by the model to reach a decision. This is crucial in fields like healthcare, finance, and law, where understanding the rationale behind decisions is vital. At Rapid Innovation, we prioritize transparency in our AI solutions, ensuring that our clients can trust the insights generated by their models.
- Common Techniques:
- LIME (Local Interpretable Model-agnostic Explanations): This technique explains individual predictions by approximating the model locally with an interpretable one. Rapid Innovation employs LIME to help clients understand specific predictions, enabling them to make informed decisions based on model outputs.
- SHAP (SHapley Additive exPlanations): SHAP values provide a unified measure of feature importance, helping to understand the contribution of each feature to the prediction. By utilizing SHAP, we assist clients in identifying key factors influencing their business outcomes.
- Visualizations: Decision paths can be visualized through flowcharts or decision trees, making it easier for stakeholders to grasp complex decision-making processes. Our team at Rapid Innovation creates intuitive visualizations that facilitate stakeholder engagement and comprehension.
- Use Cases: In healthcare, for instance, decision path methods can help clinicians understand why a model predicts a certain diagnosis, thereby improving trust and adoption of AI tools. Rapid Innovation has successfully implemented these machine learning decision path methods in various healthcare projects, leading to enhanced decision-making and patient care. Additionally, our expertise in generative AI development allows us to create innovative solutions tailored to specific client needs.
8.4. Confidence Scoring and Uncertainty Communication
Confidence scoring and uncertainty communication are critical components in the deployment of machine learning models, especially in high-stakes environments.
- Confidence Scores: These scores indicate the model's certainty regarding its predictions. A higher score suggests greater confidence, while a lower score indicates uncertainty. At Rapid Innovation, we ensure that our models provide clear confidence scores, allowing clients to gauge the reliability of predictions.
- Importance of Uncertainty:
- Risk Management: Understanding uncertainty helps in risk assessment and management, allowing practitioners to make informed decisions. Our solutions empower clients to navigate uncertainties effectively, minimizing potential risks.
- Informed Decision-Making: By communicating uncertainty, stakeholders can weigh the risks and benefits of following a model's recommendation. Rapid Innovation emphasizes the importance of clear communication in our AI solutions, enhancing decision-making processes.
- Methods of Communication:
- Visual Aids: Graphs and charts can effectively convey confidence levels and uncertainties. We leverage visual aids to present complex data in an accessible manner, ensuring stakeholders can easily interpret results.
- Thresholds: Setting thresholds for action based on confidence scores can guide users on when to trust the model's predictions. Our team collaborates with clients to establish appropriate thresholds tailored to their specific needs.
- Applications: In clinical settings, for example, a model predicting patient outcomes might provide a confidence score that helps doctors decide whether to proceed with a particular treatment. Rapid Innovation has developed models that integrate confidence scoring, leading to improved clinical decision-making.
8.5. Clinical Validation of Explanations
Clinical validation of explanations is a crucial step in ensuring that machine learning models are not only accurate but also interpretable and trustworthy in real-world applications.
- Importance of Validation:
- Trust: Clinicians and patients need to trust the explanations provided by AI systems to adopt them in practice. Rapid Innovation focuses on building trust through rigorous validation processes.
- Safety: Validated explanations can prevent harmful decisions based on incorrect interpretations of model outputs. Our commitment to safety ensures that our clients can rely on the AI solutions we provide.
- Methods of Validation:
- User Studies: Conducting studies with healthcare professionals to assess the clarity and usefulness of explanations. We facilitate user studies to gather feedback and refine our models, ensuring they meet the needs of end-users.
- Comparative Analysis: Comparing model explanations with expert opinions to evaluate their accuracy and reliability. Rapid Innovation employs comparative analysis to enhance the credibility of our AI solutions.
- Regulatory Considerations: Regulatory bodies may require evidence of clinical validation before approving AI tools for use in healthcare settings. Our expertise in navigating regulatory landscapes helps clients achieve compliance efficiently.
- Real-World Impact: Validated explanations can lead to better patient outcomes by ensuring that healthcare providers understand the reasoning behind AI recommendations, ultimately enhancing the quality of care. Rapid Innovation is dedicated to delivering AI solutions that not only meet regulatory standards but also drive meaningful improvements in healthcare delivery.
9. Implementation and Deployment
The implementation and deployment phase is crucial for the success of any health information system, including electronic health record implementation and electronic medical records implementation. This stage involves setting up the necessary technical infrastructure and ensuring seamless integration with existing health information systems.
9.1 Technical Infrastructure Requirements
Establishing a robust technical infrastructure is essential for the effective functioning of health information systems. Key requirements include:
- Hardware Specifications:
- Servers: High-performance servers are needed to handle data processing and storage.
- Workstations: Reliable computers for healthcare professionals to access the system.
- Networking Equipment: Routers, switches, and firewalls to ensure secure and efficient data transmission.
- Software Requirements:
- Operating Systems: Compatible operating systems that support the health information system.
- Database Management Systems: Efficient databases to store and manage patient data securely.
- Security Software: Antivirus and encryption tools to protect sensitive health information.
- Cloud Infrastructure:
- Consideration of cloud-based solutions for scalability and flexibility.
- Ensuring compliance with regulations such as HIPAA for data security.
- Backup and Recovery Solutions:
- Regular data backups to prevent loss of critical information.
- Disaster recovery plans to restore operations quickly in case of system failures.
- User Access and Authentication:
- Role-based access controls to ensure that only authorized personnel can access sensitive data.
- Multi-factor authentication for enhanced security.
- Training and Support:
- Comprehensive training programs for staff to familiarize them with the new system, including resources needed for ehr implementation.
- Ongoing technical support to address any issues that arise post-deployment.
9.2 Integration with Existing Health Information Systems
Integrating new health information systems with existing ones is vital for ensuring continuity of care and data consistency. Key considerations include:
- Interoperability Standards:
- Adopting standards such as HL7 or FHIR to facilitate data exchange between systems.
- Ensuring that the new system can communicate effectively with legacy systems.
- Data Migration:
- Planning for the transfer of existing patient data to the new system, which is a critical aspect of implementing electronic health records in hospitals.
- Validating data integrity during the migration process to avoid discrepancies.
- API Development:
- Creating application programming interfaces (APIs) to enable seamless communication between different systems.
- Ensuring that APIs are secure and efficient to handle data requests.
- Stakeholder Collaboration:
- Engaging with all stakeholders, including healthcare providers, IT staff, and patients, to gather input and address concerns.
- Establishing a governance framework to oversee integration efforts.
- Testing and Validation:
- Conducting thorough testing to ensure that the new system works well with existing systems, including the implementation of hospital information systems.
- Validating that data flows correctly and that users can access the information they need.
- Change Management:
- Implementing strategies to manage the transition to the new system, including an ehr implementation plan and ehr implementation timeline.
- Communicating changes effectively to all users to minimize resistance and confusion.
- Continuous Monitoring and Improvement:
- Setting up monitoring tools to track system performance and user satisfaction.
- Regularly updating the system based on feedback and technological advancements.
By focusing on these technical infrastructure requirements and integration strategies, healthcare organizations can ensure a successful implementation and deployment of their health information systems. Rapid Innovation is committed to guiding clients through this process, leveraging our AI expertise to enhance operational efficiency and ultimately improve patient care outcomes. Our tailored solutions not only streamline implementation but also maximize return on investment by ensuring that systems are optimized for performance and user satisfaction, including the cost of implementing electronic health records and electronic medical records. For insights on the future of AI in healthcare, check out our article on AI Knowledge Management.
9.3. Deployment Models (Cloud, On-Premise, Hybrid)

Deployment models are crucial in determining how an organization utilizes its IT resources. The three primary deployment models are cloud, on-premise, and hybrid.
- Cloud Deployment: Resources are hosted on the cloud provider's infrastructure, offering flexibility and scalability that allows businesses to pay for what they use. This model is ideal for organizations looking to reduce capital expenditure and improve accessibility. Rapid Innovation can assist clients in leveraging cloud deployment to enhance operational efficiency and drive innovation, ultimately leading to greater ROI. Various cloud deployment models, such as private cloud deployment model and community cloud example, can be tailored to meet specific organizational needs.
- On-Premise Deployment: All resources are hosted within the organization’s own data center, providing greater control over data security and compliance. This model requires significant upfront investment in hardware and software and is suitable for businesses with strict regulatory requirements or those that need to maintain sensitive data internally. Rapid Innovation can guide clients in optimizing their on-premise solutions to ensure they meet compliance standards while maximizing performance.
- Hybrid Deployment: This model combines both cloud and on-premise resources, offering flexibility to move workloads between environments as needed. It allows organizations to leverage the benefits of both models, optimizing costs and performance. Hybrid deployment is ideal for businesses that require scalability but also need to keep certain data on-premise for compliance reasons. Rapid Innovation can help clients design and implement hybrid solutions that align with their strategic goals, ensuring they achieve the best of both worlds. Understanding the different cloud computing deployment models is essential for organizations to make informed decisions. Additionally, for organizations looking to enhance their AI capabilities, Rapid Innovation offers specialized services in transformer model development.
Each deployment model has its advantages and disadvantages, and the choice depends on the specific needs and goals of the organization.
10. Clinical Testing and Validation
Clinical testing and validation are crucial steps in the development of any medical product or treatment. These processes ensure that the product is safe, effective, and meets regulatory standards before it reaches the market. At Rapid Innovation, we leverage advanced AI technologies to streamline these processes, enhancing efficiency and accuracy, which ultimately leads to greater ROI for our clients.
10.1 Pilot Study Design
Pilot studies are preliminary investigations conducted to test the feasibility, time, cost, and adverse events involved in a larger clinical trial. They serve as a critical step in the clinical testing process.
- Purpose of Pilot Studies:
- Assess the practicality of the study design.
- Identify potential issues in the methodology.
- Gather preliminary data to inform larger studies.
- Key Components of Pilot Study Design:
- Sample Size: Typically smaller than full-scale trials, often involving 10-30 participants.
- Objectives: Clearly defined goals, such as testing recruitment strategies or measuring outcome variability.
- Methodology: Detailed protocols for data collection, participant monitoring, and analysis.
- Benefits of Pilot Studies:
- Helps refine the study design before full-scale implementation.
- Provides insights into participant recruitment and retention strategies.
- Identifies logistical challenges that may arise during the main trial.
- Challenges in Pilot Study Design:
- Limited generalizability due to small sample sizes.
- Potential for bias if not properly randomized.
- Difficulty in measuring long-term outcomes.
Pilot studies are essential for minimizing risks and ensuring that larger clinical trials are well-structured and capable of yielding valid results. Rapid Innovation employs AI-driven analytics to enhance pilot study design, allowing for more precise data collection and analysis, which can significantly reduce costs and time to market. This is particularly important in the context of clia validation and clia validation requirements, ensuring that all clinical testing adheres to necessary standards.
10.2 Multi-center Clinical Trials

Multi-center clinical trials involve conducting research at multiple locations or institutions. This approach enhances the diversity of the participant pool and increases the generalizability of the findings.
- Advantages of Multi-center Trials:
- Diverse Population: Access to a broader demographic, which can improve the applicability of results.
- Increased Recruitment: More sites can lead to faster participant enrollment.
- Resource Sharing: Collaboration among institutions can lead to shared expertise and resources.
- Design Considerations:
- Standardization: Protocols must be standardized across all sites to ensure consistency in data collection and analysis.
- Coordination: Effective communication and coordination among sites are essential to manage logistics and data integrity.
- Regulatory Compliance: Each site must adhere to local regulations and ethical guidelines, which can vary by location, including compliance with clia assay validation requirements.
- Challenges in Multi-center Trials:
- Variability in Data: Differences in patient populations and practices can introduce variability in results.
- Complexity in Management: Coordinating multiple sites can complicate logistics and increase administrative burdens.
- Funding and Resources: Securing adequate funding to support multiple sites can be challenging.
Multi-center clinical trials are vital for validating the efficacy and safety of medical interventions across diverse populations, ultimately leading to more robust and reliable outcomes. Rapid Innovation's expertise in AI can facilitate the management of multi-center trials by automating data collection and analysis, ensuring consistency and compliance across all sites, which enhances the overall quality of the research and maximizes ROI for our clients. This includes adherence to clia ngs validation and clia validation guidelines, ensuring that all clinical testing and validation processes meet the highest standards. For more information on our services, visit our AI Agent Clinical Trial Optimization Assistant page.
10.3. Comparative Analysis with Traditional Diagnostics
In the realm of medical diagnostics, traditional methods have long been the standard. However, advancements in technology have introduced modern diagnostic tools that offer various advantages. A comparative analysis between traditional diagnostics and modern techniques reveals several key differences:
- Accuracy and Precision: Modern diagnostic tools often provide higher accuracy and precision compared to traditional methods. For instance, molecular diagnostics can detect diseases at a genetic level, which traditional methods may miss, leading to more targeted and effective treatments.
- Speed of Results: Traditional diagnostics can take days or even weeks to yield results. In contrast, newer technologies, such as point-of-care testing, can deliver results in real-time, significantly improving patient management and enabling timely interventions.
- Cost-Effectiveness: While some modern diagnostic tools may have higher upfront costs, they can lead to cost savings in the long run by reducing the need for multiple tests and hospitalizations, ultimately enhancing the return on investment for healthcare providers.
- Patient Experience: Newer diagnostic methods often require less invasive procedures, enhancing patient comfort and satisfaction. For example, blood tests can replace more invasive biopsies in certain cases, leading to a more positive patient experience.
- Integration with Technology: Modern diagnostics often integrate with electronic health records (EHR), allowing for seamless data sharing and improved patient care coordination, which is essential for efficient healthcare delivery. Additionally, the integration of blockchain technology in healthcare can enhance security and transparency in patient data management, as seen in blockchain banking solutions and in AI's leap in advanced image analysis.
10.4. Time-to-Diagnosis Impact Assessment
Time-to-diagnosis is a critical factor in patient outcomes. Delays in diagnosis can lead to disease progression, increased treatment costs, and poorer prognoses. Assessing the impact of time-to-diagnosis involves several considerations:
- Disease Severity: Certain conditions, such as cancer, require prompt diagnosis for effective treatment. Delays can lead to advanced stages of disease, complicating treatment options and negatively impacting patient outcomes.
- Patient Outcomes: Studies have shown that faster diagnosis correlates with better clinical outcomes. For instance, early detection of diseases like sepsis can significantly reduce mortality rates, demonstrating the importance of timely diagnostics.
- Healthcare Costs: Delayed diagnoses can lead to increased healthcare costs due to the need for more extensive treatments and longer hospital stays. A study indicated that timely diagnosis could save the healthcare system billions annually, highlighting the financial benefits of efficient diagnostic processes.
- Patient Satisfaction: Quick diagnosis not only improves clinical outcomes but also enhances patient satisfaction. Patients who receive timely information about their health are more likely to trust their healthcare providers, fostering a better patient-provider relationship.
- Workflow Efficiency: Streamlining the diagnostic process can improve overall healthcare efficiency. Reducing time-to-diagnosis allows healthcare providers to manage more patients effectively, optimizing resource allocation.
10.5. Clinical Outcome Measures
Clinical outcome measures are essential for evaluating the effectiveness of diagnostic methods and treatments. These measures provide insights into patient health and the overall quality of care:
- Survival Rates: One of the most critical clinical outcome measures is the survival rate of patients diagnosed with specific conditions. Higher survival rates often indicate effective diagnostic and treatment protocols, reinforcing the value of advanced diagnostics.
- Quality of Life: Assessing the quality of life post-diagnosis is vital. Patients who receive timely and accurate diagnoses often report better quality of life due to effective management of their conditions, which is a key indicator of successful healthcare delivery.
- Functional Status: Measuring a patient’s functional status post-treatment can indicate the success of diagnostic methods. Improved functional status suggests that the diagnosis led to effective interventions, contributing to better overall health outcomes.
- Recurrence Rates: For chronic conditions, monitoring recurrence rates is crucial. Lower recurrence rates can signify that the initial diagnosis and subsequent treatment were effective, demonstrating the importance of accurate diagnostics.
- Patient-Reported Outcomes: Gathering data on patient-reported outcomes can provide valuable insights into the effectiveness of diagnostic methods. These outcomes reflect the patient's perspective on their health status and treatment efficacy, which is essential for continuous improvement in healthcare practices.
11. Regulatory and Compliance Framework
The regulatory and compliance framework is crucial for ensuring that medical devices and pharmaceuticals are safe, effective, and meet the necessary standards before they reach the market. This framework varies by region, with the FDA in the United States and CE marking in Europe being two of the most significant regulatory pathways.
11.1 FDA Approval Pathways
The U.S. Food and Drug Administration (FDA) oversees the approval of medical devices and pharmaceuticals through several pathways, each designed to address different types of products and their associated risks. Understanding these pathways is essential for manufacturers aiming to bring their products to market.
- Premarket Notification (510(k)): This pathway is for devices that are substantially equivalent to an already marketed device. Manufacturers must demonstrate that their device is as safe and effective as the predicate device.
- Premarket Approval (PMA): This is a more rigorous process for high-risk devices. Manufacturers must provide clinical data to support the safety and effectiveness of their device.
- De Novo Classification: This pathway is for novel devices that are low to moderate risk and do not have a predicate. It allows for a streamlined process to classify new devices and establish regulatory controls.
- Humanitarian Device Exemption (HDE): This is for devices intended to treat or diagnose conditions affecting fewer than 8,000 individuals per year in the U.S. It allows for approval based on a reasonable assurance of safety and probable benefit rather than effectiveness.
- Breakthrough Devices Program: This program is designed to expedite the development and review of devices that provide more effective treatment or diagnosis of life-threatening or irreversibly debilitating diseases.
Each pathway has specific requirements and timelines, making it essential for manufacturers to choose the appropriate route based on their product's classification and intended use. Rapid Innovation can assist clients in navigating these pathways efficiently, leveraging AI-driven analytics to streamline documentation and compliance processes, ultimately reducing time-to-market and enhancing ROI. This includes understanding medical device compliance standards and ensuring adherence to FDA medical device compliance regulations.
11.2 CE Marking Requirements
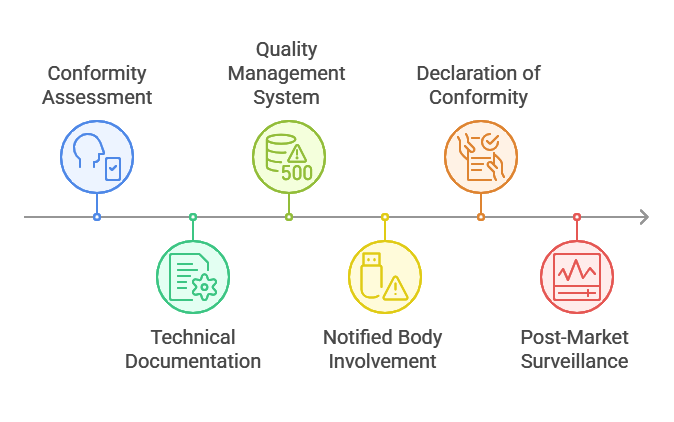
CE marking is a certification mark that indicates conformity with health, safety, and environmental protection standards for products sold within the European Economic Area (EEA). It is essential for manufacturers looking to market their medical devices in Europe.
- Conformity Assessment: Manufacturers must conduct a conformity assessment to ensure their device meets the essential requirements outlined in the Medical Device Regulation (MDR) or In Vitro Diagnostic Regulation (IVDR). This includes compliance with the european mdr regulation and ivdr regulation compliance.
- Technical Documentation: A comprehensive technical file must be prepared, including device description and specifications, design and manufacturing processes, risk management and clinical evaluation data, and labeling and instructions for use.
- Quality Management System (QMS): Manufacturers must implement a QMS compliant with ISO 13485, which outlines the requirements for a comprehensive quality management system for the design and manufacture of medical devices. This is part of the broader medical device quality assurance and regulatory compliance framework.
- Notified Body Involvement: For higher-risk devices, a Notified Body must be involved in the conformity assessment process. They will review the technical documentation and may conduct audits of the manufacturer’s QMS, ensuring that medical device regulatory compliance is met.
- Declaration of Conformity: Once compliance is established, manufacturers must draft a Declaration of Conformity, stating that their device meets all relevant EU legislation.
- Post-Market Surveillance: After obtaining CE marking, manufacturers are required to monitor the device's performance in the market and report any adverse events. This is part of the ongoing medical device compliance and medical equipment regulatory compliance efforts.
CE marking is a critical step for manufacturers aiming to access the European market, ensuring that their products meet stringent safety and performance standards. Rapid Innovation can provide tailored consulting services to help clients prepare for CE marking, utilizing AI tools to enhance compliance tracking and documentation accuracy, thereby maximizing their market potential and ROI. This includes support for crypto token development and ensuring adherence to 21 cfr 820 compliance and fda qsr compliance, as well as utilizing AI agents for predictive device failure detection.
11.3. HIPAA and GDPR Compliance
HIPAA (Health Insurance Portability and Accountability Act) and GDPR (General Data Protection Regulation) are two critical regulations that govern the handling of personal health information. Understanding their compliance requirements is essential for healthcare organizations and technology providers.
- HIPAA focuses on protecting patient information in the United States. It mandates that healthcare providers, insurers, and their business associates implement safeguards to ensure the confidentiality, integrity, and availability of protected health information (PHI). Key components of HIPAA include:
- Privacy Rule: Establishes standards for the protection of PHI.
- Security Rule: Outlines the physical, administrative, and technical safeguards required to protect electronic PHI.
- Breach Notification Rule: Requires covered entities to notify individuals of breaches of unsecured PHI.
- GDPR, on the other hand, is a comprehensive data protection regulation in the European Union. It emphasizes the rights of individuals regarding their personal data and imposes strict obligations on organizations that process this data. Key components of GDPR include:
- Consent: Organizations must obtain explicit consent from individuals before processing their data.
- Right to Access: Individuals have the right to access their personal data and understand how it is being used.
- Data Protection by Design: Organizations must implement data protection measures from the outset of any project involving personal data.
- Compliance with both HIPAA and GDPR can be challenging for organizations operating in both the U.S. and Europe. Key considerations include:
- Data Transfer: Organizations must ensure that any transfer of data between the U.S. and EU complies with both regulations.
- Risk Assessment: Regular risk assessments are necessary to identify vulnerabilities and ensure compliance with healthcare compliance regulations.
- Training: Staff must be trained on both HIPAA and GDPR requirements to ensure adherence to regulations, including hipaa guidelines for healthcare professionals.
At Rapid Innovation, we leverage our expertise in AI to help healthcare organizations navigate these complex compliance landscapes. By implementing AI-driven solutions, we can automate risk assessments and enhance data protection measures, ultimately leading to greater efficiency and reduced compliance costs. Our services include tailored AI insurance solutions that can further support compliance efforts, including AI agents for compliance monitoring.
11.4. Clinical Decision Support Software Regulations
Clinical Decision Support Software (CDSS) plays a vital role in enhancing patient care by providing healthcare professionals with evidence-based recommendations. However, the regulation of CDSS is crucial to ensure safety and efficacy.
- The FDA (Food and Drug Administration) in the U.S. regulates CDSS under the category of medical devices. The classification of CDSS depends on its intended use and the level of risk it poses to patients. Key regulatory considerations include:
- Software Classification: CDSS can be classified as Class I, II, or III devices, with Class III requiring the most stringent regulatory oversight.
- Pre-market Approval: Some CDSS may require pre-market approval (PMA) or 510(k) clearance, depending on their intended use and risk level.
- Post-market Surveillance: Once approved, CDSS must undergo post-market surveillance to monitor its performance and safety in real-world settings.
- In addition to FDA regulations, organizations must also consider:
- HIPAA Compliance: CDSS must comply with HIPAA regulations to protect patient data, including healthcare compliance laws and regulations.
- Interoperability Standards: CDSS should adhere to interoperability standards to ensure seamless integration with electronic health records (EHRs) and other health IT systems.
- Clinical Validation: CDSS must be clinically validated to ensure that its recommendations are based on sound evidence and improve patient outcomes.
Rapid Innovation can assist in developing CDSS that not only meets regulatory requirements but also enhances clinical workflows through AI-driven insights, ultimately improving patient outcomes and increasing ROI for healthcare providers.
11.5. International Regulatory Considerations
As healthcare technology continues to evolve, international regulatory considerations become increasingly important for organizations operating globally. Different countries have varying regulations that impact the development and deployment of healthcare technologies.
- Key international regulations include:
- CE Marking: In Europe, medical devices, including software, must obtain CE marking to demonstrate compliance with the Medical Device Regulation (MDR).
- TGA Approval: In Australia, the Therapeutic Goods Administration (TGA) regulates medical devices and software, requiring compliance with local standards.
- Health Canada: In Canada, medical devices must comply with the Medical Devices Regulations, which include safety and effectiveness requirements.
- Organizations must navigate these regulations by:
- Conducting Market Research: Understanding the regulatory landscape in each target market is essential for compliance, including regulatory compliance in healthcare organizations.
- Engaging Local Experts: Collaborating with local regulatory experts can help organizations navigate complex regulations and ensure compliance with regulatory requirements in healthcare.
- Adapting Products: Organizations may need to adapt their products to meet the specific regulatory requirements of each country, including healthcare compliance laws.
- Additionally, organizations should consider:
- Data Privacy Laws: Different countries have varying data privacy laws that may impact how patient data is collected, stored, and processed, including hipaa rules in healthcare.
- Cultural Differences: Understanding cultural differences in healthcare practices can influence the acceptance and effectiveness of healthcare technologies.
- Global Collaboration: Engaging in global collaborations can help organizations stay informed about international regulatory changes and best practices.
At Rapid Innovation, we provide consulting services that help organizations understand and comply with international regulations, ensuring that their healthcare technologies are not only innovative but also compliant and market-ready. Our AI solutions can streamline compliance processes, ultimately leading to enhanced operational efficiency and improved ROI.
12. Ethical Dimensions
The ethical dimensions of healthcare technology and practices are crucial in ensuring that patient rights and dignity are upheld. This section explores two significant aspects: patient consent and autonomy, and bias detection and mitigation.
12.1 Patient Consent and Autonomy
Patient consent and autonomy are foundational principles in healthcare ethics. They emphasize the importance of respecting individuals' rights to make informed decisions about their own medical care, which is a key aspect of ethics in medical practice.
Patients must be provided with comprehensive information about their treatment options, including potential risks and benefits, which allows them to make educated choices regarding their health. Respecting patient autonomy means acknowledging their right to refuse or accept treatment, and healthcare providers must support patients in making decisions that align with their values and preferences. Effective communication is essential for ensuring that patients understand their options, which includes using clear language and avoiding medical jargon. Additionally, different cultures may have varying beliefs about health and decision-making; therefore, healthcare providers should be aware of these differences and respect them in the consent process.
Failure to obtain proper consent can lead to legal consequences for healthcare providers, making it vital to understand the legal framework surrounding consent for compliance and ethical practice. The ethical obligation to obtain informed consent is not just a legal requirement; it is a moral imperative that fosters trust between patients and healthcare providers. This is particularly relevant in discussions about ethical issues in healthcare and the law of medical ethics.
12.2 Bias Detection and Mitigation
Bias in healthcare can lead to disparities in treatment and outcomes. Detecting and mitigating bias is essential for promoting equity and fairness in medical practices, which is a significant ethical aspect of healthcare.
Bias can manifest in various forms, including racial, gender, and socioeconomic biases. Recognizing these biases is the first step toward addressing them. Utilizing advanced data analytics and AI-driven solutions, Rapid Innovation can help healthcare providers identify patterns of bias in treatment decisions. By analyzing patient outcomes across different demographics, we enable clients to pinpoint areas needing improvement. Ongoing training for healthcare professionals on implicit bias can enhance awareness and reduce discriminatory practices, with workshops and seminars providing valuable insights into recognizing and addressing bias, which are current ethical healthcare issues.
Promoting diversity within healthcare teams can lead to more equitable treatment decisions, as diverse perspectives can help challenge existing biases and improve patient care. Establishing clear policies that promote equity and inclusion can also help mitigate bias, and these policies should be regularly reviewed and updated to reflect best practices in healthcare ethics and law.
Addressing bias is not only an ethical obligation but also a critical component of improving healthcare outcomes for all patients. By actively working to detect and mitigate bias, healthcare providers can create a more equitable system that benefits everyone. Rapid Innovation is committed to supporting healthcare organizations in these efforts, ensuring that technology and practices align with ethical standards while enhancing overall patient care, including addressing ethical problems in healthcare and the ethical issues in the healthcare industry. For more information on how we can assist with these initiatives, visit our AI in Healthcare.
12.3. Health Disparities in Rare Disease Diagnosis

Health disparities in rare disease diagnosis refer to the unequal access to healthcare resources and diagnostic services that can lead to delayed or missed diagnoses for certain populations. These disparities can be influenced by various factors, including socioeconomic status, geographic location, and systemic biases within the healthcare system.
- Socioeconomic Factors: Individuals from lower socioeconomic backgrounds may lack access to specialized healthcare providers or genetic testing, which are crucial for diagnosing rare diseases. This can result in longer diagnostic odysseys and poorer health outcomes.
- Geographic Barriers: People living in rural or underserved areas often face challenges in accessing healthcare facilities equipped to diagnose rare diseases. Limited availability of specialists can lead to misdiagnosis or delayed diagnosis.
- Cultural and Linguistic Barriers: Language differences and cultural misunderstandings can hinder effective communication between patients and healthcare providers, impacting the quality of care and the likelihood of receiving a timely diagnosis.
- Systemic Biases: Implicit biases in the healthcare system can lead to disparities in how symptoms are interpreted based on race, gender, or age. This can result in certain groups being overlooked or misdiagnosed.
Addressing these disparities requires a multifaceted approach, including increased funding for research on rare diseases, improved access to genetic testing, and training for healthcare providers to recognize and address biases in diagnosis. At Rapid Innovation, we leverage AI-driven solutions to analyze healthcare data, identify patterns, and provide insights that can help organizations target interventions effectively, ultimately improving access to diagnostic services for underserved populations. Additionally, our Robotic Process Automation solutions can streamline processes and enhance efficiency in healthcare delivery.
12.4. Algorithmic Accountability
Algorithmic accountability refers to the responsibility of developers and organizations to ensure that algorithms used in healthcare and other sectors are transparent, fair, and effective. As algorithms increasingly influence decision-making processes, particularly in healthcare, the need for accountability becomes paramount.
- Transparency: It is essential for organizations to disclose how algorithms are developed and the data used in their training. This transparency helps stakeholders understand the potential biases and limitations of the algorithms.
- Bias Mitigation: Algorithms can inadvertently perpetuate existing biases if not carefully monitored. Regular audits and assessments are necessary to identify and rectify biases in algorithmic decision-making, ensuring equitable outcomes for all patients.
- Stakeholder Engagement: Involving diverse stakeholders, including patients, healthcare providers, and ethicists, in the development and evaluation of algorithms can enhance accountability. This collaborative approach can help ensure that algorithms meet the needs of various populations.
- Regulatory Frameworks: Establishing regulatory guidelines for algorithmic use in healthcare can promote accountability. These frameworks can set standards for data privacy, algorithmic transparency, and bias mitigation.
By prioritizing algorithmic accountability, healthcare organizations can enhance trust in technology and ensure that algorithms contribute positively to patient care. Rapid Innovation specializes in developing robust AI algorithms that prioritize transparency and fairness, ensuring that our clients can trust the technology they implement.
12.5. Balancing Automation with Human Expertise
Balancing automation with human expertise is crucial in healthcare, particularly as technology continues to evolve. While automation can enhance efficiency and accuracy, human expertise remains essential for nuanced decision-making and patient care.
- Complementary Roles: Automation can handle repetitive tasks, such as data entry and preliminary analysis, allowing healthcare professionals to focus on complex cases that require critical thinking and empathy.
- Decision Support: Automated systems can provide decision support tools that assist healthcare providers in diagnosing and treating patients. However, these tools should be used to augment, not replace, human judgment.
- Training and Education: As automation becomes more prevalent, ongoing training for healthcare professionals is vital. This ensures that they can effectively interpret automated outputs and integrate them into their clinical practice.
- Patient-Centered Care: Human expertise is essential for maintaining a patient-centered approach. Healthcare providers must engage with patients, understand their unique circumstances, and make decisions that consider their preferences and values.
- Ethical Considerations: The integration of automation raises ethical questions about accountability and the potential for dehumanization in care. It is crucial to maintain a balance that prioritizes patient welfare and ethical standards.
By effectively balancing automation with human expertise, healthcare systems can leverage technology to improve outcomes while ensuring that the human touch remains at the forefront of patient care. At Rapid Innovation, we provide consulting services that help organizations implement AI solutions while maintaining the essential human elements of care, ensuring that technology enhances rather than replaces the invaluable expertise of healthcare professionals.
13. Continuous Learning and Improvement
Continuous learning and improvement are essential components in any field, especially in data science and machine learning. These practices ensure that models remain relevant, accurate, and effective over time. By implementing a structured approach to continuous learning in data science and improvement, organizations can adapt to changing environments and maintain a competitive edge.
13.1 Feedback Loop Implementation

A feedback loop is a systematic process that allows organizations to gather insights from the performance of their models and use that information to make informed adjustments. Implementing a feedback loop involves several key steps:
- Data Collection: Regularly collect data on model performance, including accuracy, precision, recall, and other relevant metrics. This data can come from user interactions, system outputs, or external sources.
- Analysis: Analyze the collected data to identify patterns, trends, and areas for improvement. This analysis can help pinpoint specific weaknesses in the model or highlight successful features that should be enhanced.
- Adjustment: Based on the analysis, make necessary adjustments to the model. This could involve retraining the model with new data, tweaking algorithms, or modifying input features to improve performance.
- Deployment: After adjustments are made, redeploy the updated model into the production environment. Ensure that the deployment process is smooth to minimize disruptions.
- Monitoring: Continuously monitor the model's performance post-deployment. This ongoing observation is crucial for identifying any new issues that may arise and for ensuring that the model remains effective.
- User Feedback: Incorporate user feedback into the loop. Engaging with end-users can provide valuable insights that quantitative data may not reveal.
Implementing a feedback loop not only enhances model performance but also fosters a culture of continuous improvement within the organization. It encourages teams to be proactive rather than reactive, leading to better decision-making and more robust models.
13.2 Model Drift Detection
Model drift refers to the phenomenon where a machine learning model's performance degrades over time due to changes in the underlying data distribution. Detecting model drift is crucial for maintaining the accuracy and reliability of predictive models. Here are some strategies for effective model drift detection:
- Monitoring Performance Metrics: Regularly track key performance metrics such as accuracy, F1 score, and AUC-ROC. A significant drop in these metrics can indicate potential drift.
- Statistical Tests: Use statistical tests to compare the distribution of incoming data with the training data. Techniques like the Kolmogorov-Smirnov test or Chi-square test can help identify shifts in data distribution.
- Data Visualization: Visualize data distributions over time using tools like histograms or box plots. This can help in spotting trends or anomalies that may suggest drift.
- Thresholds and Alerts: Set thresholds for performance metrics and establish alert systems. If a model's performance falls below a certain level, it can trigger an alert for further investigation.
- Retraining Schedule: Establish a regular retraining schedule based on the frequency of data changes. This proactive approach can help mitigate the effects of drift before they significantly impact model performance.
- Version Control: Implement version control for models. Keeping track of different model versions allows for easier rollback to previous versions if a new model underperforms due to drift.
By effectively detecting model drift, organizations can take timely actions to retrain or adjust their models, ensuring that they continue to deliver accurate predictions. This proactive approach not only enhances model reliability but also builds trust among stakeholders who rely on these models for decision-making.
At Rapid Innovation, we specialize in integrating these continuous learning and improvement strategies into our AI solutions. By leveraging our expertise, clients can achieve greater ROI through enhanced model performance and reliability, ultimately driving better business outcomes. For more insights on the differences between MLOps and DevOps, check out our article on MLOps vs DevOps.
13.3. New Disease Integration Process
The New Disease Integration Process is crucial for ensuring that healthcare systems can effectively respond to emerging health threats. This process involves several key steps:
- Identification of new diseases: Continuous surveillance and research are essential to identify new diseases as they emerge. This includes monitoring global health trends and outbreaks.
- Assessment of impact: Once a new disease is identified, its potential impact on public health must be assessed. This includes understanding transmission methods, severity, and population vulnerability.
- Integration into existing frameworks: New diseases must be integrated into existing healthcare frameworks, including treatment protocols, vaccination programs, and public health policies. This ensures a coordinated response, which is part of integrating the healthcare enterprise workflow model.
- Training and education: Healthcare professionals need training on new diseases to provide effective care. This includes understanding symptoms, treatment options, and preventive measures.
- Collaboration with stakeholders: Engaging with various stakeholders, including government agencies, NGOs, and the private sector, is vital for a comprehensive response to new diseases.
The integration process is dynamic and requires ongoing evaluation to adapt to new information and changing circumstances. Rapid Innovation can assist healthcare organizations in this process by leveraging AI-driven analytics to enhance disease identification and impact assessment, ensuring a more agile and informed response to emerging health threats.
13.4. Literature Monitoring and Knowledge Updates
Literature monitoring and knowledge updates are essential for maintaining the relevance and effectiveness of healthcare practices. This process involves:
- Regular review of scientific literature: Healthcare professionals must stay updated on the latest research findings, clinical trials, and treatment guidelines. This ensures that they are using the most current information in their practice.
- Utilization of databases and journals: Accessing reputable databases and journals allows healthcare providers to find relevant studies and reviews. This can include platforms like PubMed, Cochrane Library, and others.
- Dissemination of knowledge: Sharing new findings with colleagues and the broader healthcare community is crucial. This can be done through workshops, seminars, and online platforms.
- Incorporation of evidence-based practices: New knowledge should be integrated into clinical practice guidelines to improve patient outcomes. This requires a systematic approach to evaluate the quality of evidence.
- Continuous education: Ongoing education and training programs help healthcare professionals stay informed about advancements in their field.
By prioritizing literature monitoring and knowledge updates, healthcare systems can enhance their ability to provide high-quality care. Rapid Innovation can support this effort by developing AI tools that automate literature reviews and knowledge dissemination, ensuring that healthcare professionals have access to the latest information efficiently.
13.5. Performance Analytics and System Refinement
Performance analytics and system refinement are vital for improving healthcare delivery and outcomes. This process includes:
- Data collection and analysis: Gathering data on various performance metrics, such as patient outcomes, treatment efficacy, and operational efficiency, is essential. This data can be collected through electronic health records (EHRs) and patient surveys.
- Identifying areas for improvement: Analyzing performance data helps identify trends and areas needing enhancement. This can include patient wait times, readmission rates, and treatment adherence.
- Implementing changes: Based on the analysis, healthcare organizations can implement targeted interventions to address identified issues. This may involve process changes, staff training, or resource allocation.
- Monitoring outcomes: After implementing changes, it is crucial to monitor the outcomes to assess the effectiveness of the interventions. This helps determine if further adjustments are necessary.
- Continuous refinement: The healthcare landscape is constantly evolving, and systems must be refined regularly to adapt to new challenges and opportunities. This requires a culture of continuous improvement and innovation, which is integral to the healthcare integration process.
By focusing on performance analytics and system refinement, healthcare organizations can enhance their service delivery and ultimately improve patient care. Rapid Innovation can provide advanced AI solutions that facilitate real-time data analysis and performance monitoring, enabling healthcare providers to make informed decisions that lead to greater ROI and improved patient outcomes.
14. Case Studies and Clinical Impact
Case studies play a crucial role in understanding the real-world implications of medical practices and innovations. They provide insights into patient experiences, treatment outcomes, and the overall effectiveness of healthcare interventions. This section delves into two significant aspects of case studies: the reduction in diagnostic odyssey duration and the economic impact analysis.
14.1 Reduction in Diagnostic Odyssey Duration
The term "diagnostic odyssey" refers to the prolonged journey patients often experience while seeking a correct diagnosis for their medical conditions. This journey can be frustrating, costly, and emotionally taxing. Case studies have shown that certain interventions and technologies can significantly reduce this duration.
Implementing advanced diagnostic tools, such as genetic testing and artificial intelligence, has been shown to expedite the diagnostic process. For instance, a study indicated that genetic testing could reduce the time to diagnosis for rare diseases from several years to just a few months. Rapid Innovation leverages AI algorithms to analyze patient data swiftly, enabling healthcare providers to make informed decisions faster.
The formation of multidisciplinary teams in healthcare settings has proven effective in shortening the diagnostic odyssey. By bringing together specialists from various fields, patients receive comprehensive evaluations that lead to quicker diagnoses. Rapid Innovation can assist in creating collaborative platforms that facilitate communication among these teams, ensuring that patient information is shared seamlessly.
Focusing on patient-centric approaches that emphasize patient history and symptoms can lead to faster identification of conditions. Case studies highlight that when healthcare providers actively listen to patients and consider their input, the time to diagnosis can be significantly reduced. Rapid Innovation's AI-driven tools can enhance this process by analyzing patient feedback and history to identify potential conditions more rapidly.
The rise of telemedicine has also contributed to a decrease in diagnostic odyssey duration. Patients can consult specialists remotely, which can lead to quicker referrals and diagnoses without the need for extensive travel. Rapid Innovation supports telemedicine solutions that integrate AI to triage patients effectively, ensuring they receive timely care.
These strategies not only enhance patient satisfaction but also improve clinical outcomes by ensuring timely treatment.
14.2 Economic Impact Analysis
The economic impact of healthcare interventions is a critical area of study, as it helps stakeholders understand the financial implications of various medical practices. Case studies provide valuable data on how specific interventions can lead to cost savings and improved resource allocation.
Cost savings from early diagnosis often lead to more effective treatment, which can reduce long-term healthcare costs. For example, a case study showed that early intervention in chronic diseases can save healthcare systems up to 30% in treatment costs over time. Rapid Innovation's AI solutions can identify at-risk patients early, facilitating timely interventions that lead to significant cost reductions.
Reduction in hospitalizations through effective management of diseases via timely diagnosis can lead to fewer hospital admissions. Case studies have demonstrated that patients who receive prompt diagnoses are less likely to require emergency care, resulting in significant savings for both patients and healthcare providers. Rapid Innovation's predictive analytics can help healthcare providers anticipate patient needs, reducing the likelihood of hospitalizations.
The impact on productivity extends beyond healthcare costs. When patients receive timely diagnoses and treatments, they can return to work sooner, contributing to overall economic productivity. A study found that improved health outcomes can lead to a 20% increase in workforce productivity. Rapid Innovation's solutions can streamline the healthcare process, allowing patients to access care more efficiently and return to their daily activities sooner.
Understanding the resource allocation of various interventions allows healthcare systems to allocate resources more effectively. Case studies can reveal which treatments provide the best return on investment, guiding policy decisions and funding allocations. Rapid Innovation can assist healthcare organizations in analyzing resource utilization through AI-driven insights, ensuring optimal allocation of funds and resources.
By analyzing these economic factors, healthcare providers can make informed decisions that not only improve patient care but also enhance the sustainability of healthcare systems. Rapid Innovation is committed to helping clients achieve greater ROI through innovative AI solutions tailored to their specific needs.
In addition, various case study examples in healthcare, such as healthcare case studies and healthcare management case studies examples, illustrate the practical applications of these concepts. The integration of electronic health record case studies and big data in healthcare case study further emphasizes the importance of data analytics in healthcare case study. Moreover, healthcare marketing case studies and digital health case studies provide insights into the effectiveness of marketing strategies and digital interventions in improving patient outcomes. Overall, these case studies through the health care continuum highlight the critical role of evidence-based practices in enhancing healthcare delivery.
For those interested in exploring innovative solutions, Rapid Innovation offers services in virtual reality app development that can enhance patient engagement and treatment outcomes.
14.3. Patient Experience Improvements

Enhancing patient experience is a critical focus in modern healthcare. Improved patient experience leads to better health outcomes, increased patient satisfaction, and higher retention rates. Key areas of improvement include:
- Communication: Clear and empathetic communication between healthcare providers and patients fosters trust and understanding. Utilizing patient portals and telehealth options can enhance communication, allowing for more efficient interactions and timely responses to patient inquiries. This is essential for improving patient experience in healthcare.
- Accessibility: Ensuring that healthcare services are easily accessible is vital. This includes reducing wait times, offering flexible appointment scheduling, and providing transportation options for patients. AI-driven scheduling systems can optimize appointment availability, ensuring that patients receive timely care, which is crucial for increasing patient satisfaction.
- Personalization: Tailoring healthcare services to meet individual patient needs can significantly enhance their experience. This can involve personalized treatment plans and follow-up care that considers the patient's preferences and lifestyle. AI algorithms can analyze patient data to create customized care pathways, improving adherence and outcomes, ultimately leading to better patient satisfaction scores.
- Feedback Mechanisms: Implementing systems for collecting patient feedback helps healthcare providers identify areas for improvement. Surveys and focus groups can provide valuable insights into patient needs and expectations, enabling organizations to adapt their services accordingly. This is particularly important for improving patient satisfaction in hospitals.
- Technology Integration: Leveraging technology, such as mobile health apps and electronic health records, can streamline processes and improve patient engagement. These tools allow patients to access their health information and communicate with providers easily, enhancing overall satisfaction and care coordination, which contributes to a positive patient experience. Rapid Innovation offers AI EdTech solutions that can further enhance these technological integrations.
14.4. Healthcare Provider Adoption Patterns
The adoption of new technologies and practices by healthcare providers is crucial for improving patient care and operational efficiency. Understanding these patterns can help organizations strategize effectively. Key trends include:
- Early Adopters vs. Late Majority: Some healthcare providers are quick to adopt new technologies, while others may be more hesitant. Early adopters often lead the way in innovation, while the late majority may require more evidence of effectiveness before making changes. Rapid Innovation can assist organizations in identifying and addressing the barriers to adoption, ensuring a smoother transition.
- Influence of Regulations: Regulatory changes can significantly impact adoption patterns. Providers often adopt new technologies in response to government incentives or mandates aimed at improving care quality and patient safety. Our consulting services can help organizations navigate these regulations effectively.
- Cost Considerations: Financial factors play a significant role in adoption. Providers are more likely to invest in new technologies if they can demonstrate a clear return on investment, such as reduced operational costs or improved patient outcomes. Rapid Innovation can provide data-driven insights to help organizations make informed investment decisions.
- Training and Support: The availability of training and ongoing support can influence adoption rates. Providers are more likely to embrace new technologies if they feel confident in their ability to use them effectively. We offer tailored training programs to ensure that staff are well-equipped to utilize new tools.
- Collaboration and Partnerships: Collaborations between healthcare organizations, technology vendors, and academic institutions can facilitate the adoption of innovative practices. These partnerships often provide the resources and expertise needed to implement new solutions successfully, and Rapid Innovation can help forge these critical connections.
14.5. Success Stories and Lessons Learned
Examining success stories in healthcare can provide valuable insights and lessons for future initiatives. These examples highlight effective strategies and the importance of adaptability. Key takeaways include:
- Case Studies of Successful Implementations: Many healthcare organizations have successfully implemented new technologies or practices that improved patient care. For instance, a hospital that adopted telemedicine saw a significant increase in patient satisfaction and reduced readmission rates. Rapid Innovation can help replicate such successes by providing strategic guidance and technological support.
- Importance of Leadership Support: Strong leadership is crucial for driving change. Organizations with committed leaders who champion new initiatives tend to experience smoother transitions and greater overall success. Our consulting services emphasize the importance of leadership engagement in the adoption process.
- Engagement of Stakeholders: Involving all stakeholders, including patients, staff, and community members, in the planning and implementation process can lead to better outcomes. Engaged stakeholders are more likely to support changes and provide valuable feedback, which we facilitate through structured engagement strategies.
- Continuous Improvement: Successful organizations often embrace a culture of continuous improvement. Regularly assessing processes and outcomes allows for ongoing adjustments and enhancements to care delivery. Rapid Innovation promotes a data-driven approach to continuous improvement, ensuring that organizations remain agile and responsive to patient needs.
- Learning from Failures: Not every initiative will succeed, and it’s essential to learn from failures. Analyzing what went wrong can provide insights that inform future efforts and help avoid similar pitfalls. We assist organizations in conducting thorough post-implementation reviews to extract valuable lessons.
By focusing on patient experience improvements, understanding healthcare provider adoption patterns, and learning from success stories, the healthcare industry can continue to evolve and enhance the quality of care provided to patients. Rapid Innovation stands ready to support organizations in achieving these goals through our expertise in AI development and consulting solutions, ultimately leading to improved patient satisfaction and better patient experience in healthcare.
15. Future Directions and Research
The field of technology and healthcare is rapidly evolving, leading to exciting future directions and research opportunities. Two significant areas of focus are the healthcare technology integration with emerging diagnostic technologies and the development of advanced multimodal learning architectures.
15.1 Integration with Emerging Diagnostic Technologies

The integration of advanced diagnostic technologies into healthcare systems is crucial for improving patient outcomes and streamlining processes. This healthcare technology integration can enhance the accuracy and efficiency of diagnoses, leading to better treatment plans. Key areas of focus include:
- Artificial Intelligence (AI) and Machine Learning (ML): AI and ML algorithms can analyze vast amounts of data from various diagnostic tools, such as imaging, genomics, and lab tests, leading to more accurate and timely diagnoses. Rapid Innovation specializes in developing tailored AI solutions that help healthcare providers leverage these technologies to achieve significant improvements in diagnostic accuracy and operational efficiency.
- Wearable Health Devices: The rise of wearable technology allows for continuous monitoring of patients' health metrics. Integrating data from these devices with traditional diagnostic methods can provide a more comprehensive view of a patient's health. Rapid Innovation can assist clients in creating platforms that seamlessly aggregate and analyze this data, enhancing patient care and engagement.
- Telemedicine: The integration of telemedicine with diagnostic technologies enables remote consultations and diagnostics, making healthcare more accessible, especially in underserved areas. Our consulting services can guide organizations in implementing effective telemedicine solutions that optimize patient interactions and streamline workflows.
- Point-of-Care Testing: Emerging diagnostic technologies that allow for rapid testing at the point of care can significantly reduce the time between diagnosis and treatment, improving patient outcomes. Rapid Innovation can help clients develop and integrate these technologies into their existing systems, ensuring a smooth transition and maximizing ROI.
- Data Interoperability: Ensuring that different diagnostic technologies can communicate and share data seamlessly is essential for creating a holistic view of patient health. Our expertise in AI-driven data integration solutions can help organizations achieve interoperability, leading to better-informed clinical decisions.
Research indicates that the integration of these technologies can improve diagnostic accuracy by up to 20% in certain fields, such as radiology.
15.2 Advanced Multimodal Learning Architectures
Advanced multimodal learning architectures represent a significant leap in how we process and analyze data from various sources. These architectures can combine information from different modalities, such as text, images, and audio, to create a more nuanced understanding of complex data. The benefits include:
- Enhanced Data Fusion: By integrating data from multiple sources, multimodal learning can provide richer insights. For example, combining imaging data with patient history can lead to more accurate diagnoses. Rapid Innovation can develop custom multimodal solutions that empower healthcare providers to harness the full potential of their data.
- Improved Predictive Analytics: Multimodal architectures can enhance predictive models by incorporating diverse data types, leading to better forecasting of patient outcomes and disease progression. Our AI solutions can help clients build robust predictive models that drive proactive healthcare strategies.
- Natural Language Processing (NLP): Integrating NLP with other modalities can help in extracting valuable insights from unstructured data, such as clinical notes and research articles, thereby improving decision-making processes. Rapid Innovation offers NLP solutions that enable healthcare organizations to unlock insights from their textual data, enhancing clinical workflows.
- Robustness and Generalization: Advanced multimodal learning architectures can improve the robustness of models, making them more adaptable to different datasets and reducing the risk of overfitting. Our expertise ensures that clients benefit from models that perform well across various scenarios.
- Real-World Applications: These architectures can be applied in various fields, including personalized medicine, where they can tailor treatment plans based on a comprehensive analysis of patient data. Rapid Innovation can assist organizations in implementing these advanced architectures to deliver personalized care effectively.
Research indicates that multimodal learning can outperform single-modality approaches by up to 30% in specific tasks, such as emotion recognition.
The future of healthcare and technology lies in the seamless healthcare technology integration of these emerging diagnostic technologies and advanced multimodal learning architectures, paving the way for more effective and personalized patient care. Rapid Innovation is committed to helping clients navigate this evolving landscape, ensuring they achieve their business goals efficiently and effectively. For those interested in enhancing their services, our ChatGPT integration services can provide valuable support.
15.3. Real-time Diagnostic Capabilities
Real-time diagnostic capabilities are revolutionizing the healthcare landscape by enabling immediate analysis and decision-making. This advancement is particularly significant in critical care settings where timely interventions can save lives.
- Instant results: Technologies such as point-of-care testing and telemedicine allow healthcare providers to obtain diagnostic results almost instantaneously.
- Enhanced patient monitoring: Wearable devices and remote monitoring systems provide continuous data, allowing for real-time assessment of a patient's condition.
- Improved decision-making: With access to real-time data, clinicians can make informed decisions quickly, leading to better patient outcomes.
- Integration with AI: Artificial intelligence algorithms can analyze data in real-time, identifying patterns and anomalies that may not be immediately apparent to human clinicians. Rapid Innovation specializes in developing AI solutions that enhance real-time diagnostic capabilities, ensuring that healthcare providers can leverage data effectively for improved patient care. Additionally, advancements in telemedicine are playing a crucial role in this transformation.
- Cost-effectiveness: By reducing the time spent on diagnostics, healthcare systems can lower costs associated with prolonged hospital stays and unnecessary tests. Our consulting services help clients implement AI-driven diagnostic tools that streamline processes and maximize ROI.
15.4. Expanded Coverage of Ultra-Rare Conditions
The expansion of coverage for ultra-rare conditions is a critical development in personalized medicine. These conditions, often overlooked due to their low prevalence, are now receiving more attention from researchers and healthcare providers.
- Increased research funding: More resources are being allocated to study ultra-rare diseases, leading to better understanding and treatment options.
- Genetic testing advancements: Improved genetic testing technologies allow for the identification of rare conditions, enabling earlier diagnosis and intervention.
- Patient advocacy: Organizations dedicated to rare diseases are raising awareness and pushing for better healthcare policies and insurance coverage.
- Collaboration among stakeholders: Partnerships between pharmaceutical companies, researchers, and healthcare providers are fostering innovation in treatment options for ultra-rare conditions. Rapid Innovation can facilitate these collaborations by providing AI-driven insights that enhance research and development efforts.
- Tailored therapies: Advances in biotechnology are leading to the development of personalized therapies that target specific genetic mutations associated with rare diseases. Our expertise in AI can assist in the identification of these mutations, enabling more effective treatment strategies.
15.5. Global Accessibility and Adoption Strategies
Global accessibility and adoption strategies are essential for ensuring that healthcare innovations reach underserved populations worldwide. These strategies focus on breaking down barriers to healthcare access and promoting equitable distribution of medical resources.
- Telehealth initiatives: Expanding telehealth services can bridge the gap for patients in remote or underserved areas, providing access to specialists and essential care.
- Affordable pricing models: Developing cost-effective solutions and pricing strategies can make healthcare technologies more accessible to low-income populations.
- Training and education: Providing training for healthcare professionals in low-resource settings ensures that they can effectively use new technologies and deliver quality care. Rapid Innovation offers tailored training programs that empower healthcare workers with the skills needed to utilize AI tools effectively.
- Partnerships with local organizations: Collaborating with local health organizations can enhance the reach and effectiveness of healthcare initiatives, ensuring they are culturally appropriate and relevant.
- Policy advocacy: Engaging with policymakers to promote healthcare reforms can lead to improved access to essential services and technologies for marginalized communities. Our consulting services can support these advocacy efforts by providing data-driven insights that highlight the importance of equitable healthcare access.














.svg)